IOA Research
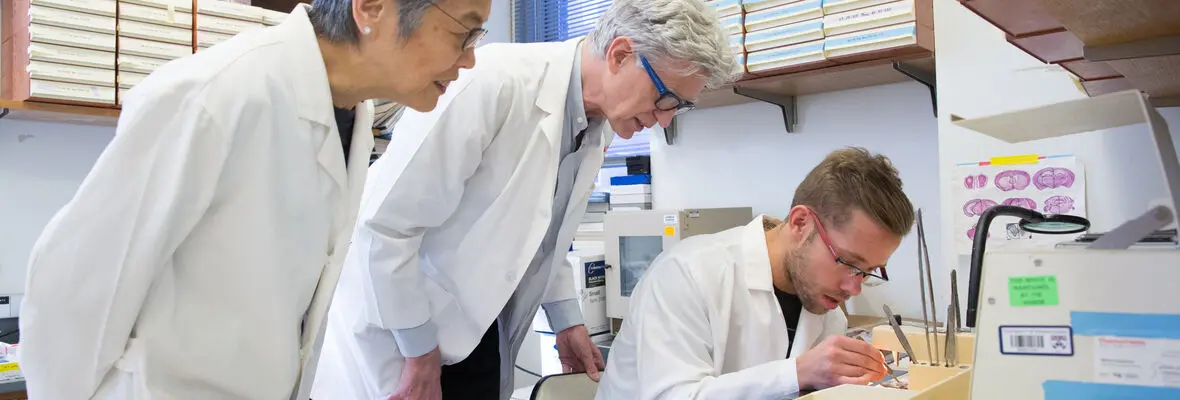
Aging Research at Penn
Through close collaborations, our Fellowship program, and our Pilot Program, the IOA collaborates with scientists, researchers, and clinicians from a variety of fields at the University of Pennsylvania. We strive to promote the continuous groundbreaking aging-related research taking place here at Penn through our educational programs, events, and funding opportunities.