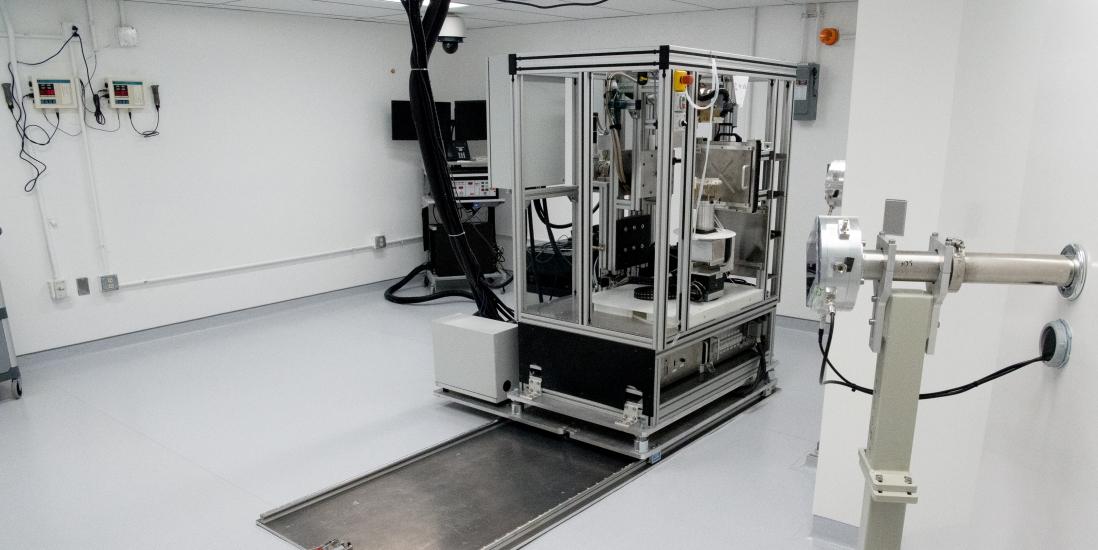
Proton SARRP on rails
Protons – Conventional and Flash Radiation Therapy
Our facility is set up for proton radiotherapy experiments using both Conventional (≈ 1Gy/s) as well as Ultra-high dose rate - FLASH (≥ 60Gy/s) Irradiation. Different stages and collimators make any setup or fixed gantry treatment possible. Customized proton arc therapy is possible using SARRP's robotic stage in combination with vertical and horizontal rodent platforms that can be rotated 360 degrees in front of the fixed proton gantry. From rodents to larger species, different treatments are possible based on field size and dose rate.
The first generation SARRP System Features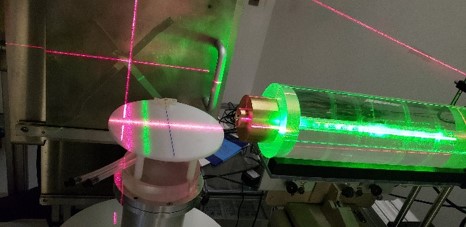
- Isocenteric targeting accuracy of 0.25 mm
- On board cone beam CT and image reconstruction
- Minimum field size of 0.5 mm in diameter
- CBCT panel for kV imaging
- 120 degree isocentric gantry rotation and robotic specimen stage enable non-coplanar field arrangements
SARRP Research Platform Advantages
- Provides state-of-the-art 3D volumetric image guidance for localization and targeting of the dose
- Conformal dose minimizes exposure to non-targeted tissues and organs
- Non-invasive procedure
- Easy to use, reliable, and reproducible
- Customizable to meet new and innovative applications
- High resolution, low imaging dose, on board CT imaging and 3D reconstruction
- Image fusion options for easy target localization and avoidance of organs at risk
- High precision beam geometry to achieve conformal dose distributions
- Open platform to enable the addition of other imaging modalities for future research
Applications
The SARRP research platform enables researchers to replicate the radiotherapy process of imaging, target localization and radiotherapy treatment delivery techniques employed when treating patients in clinical oncology departments. In order to improve the efficiency of radiation therapy and minimize the short and long term side effects of cancer treatment it is vital to study radiation biology using in vivo models.
- Radiobiology
- Preclinical studies
- DNA damage response
- Tumor biology and the micro-environment
- Bystander effects
- Radiosensitizers
- Cardiovascular toxicity
- Oncology research
- Preclinical validation of radiotherapy – assessing the risks of radiation exposure balanced against the efficacy of the treatment in controlling and eliminating tumors
- Normal tissue injury by radiotherapy
- Immunology disease
- Cardiovascular diseases
- Radiobiological effectiveness
- Characterize tumors that may not respond to ionizing radiation
- DNA damage response
- Can couple spatially targeted radiotherapy with molecularly targeted therapies to optimize treatments for solid tumors