Research Team
CBIR Leadership
-
Read More about Douglas H. Smith, MD
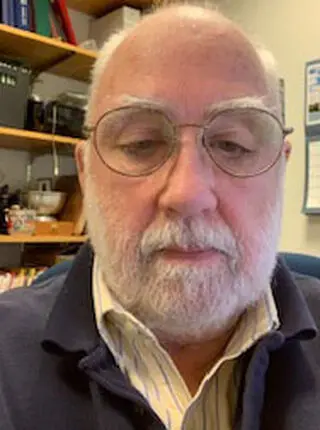
Douglas H. Smith, MD
Director, Penn Center for Brain Injury and Repair, Neurosurgery
Douglas H. Smith, MD
Director, Penn Center for Brain Injury and Repair, Neurosurgery
Douglas H. Smith Douglas H. Smith, M.D. is the Robert A. Groff Endowed Professor and Vice Chairman of Neurosurgery at the University of Pennsylvania. He also Directs Penn’s Center for Brain Injury and Repair, which includes over 30 faculty members and their research teams. In addition, Dr. Smith currently serves as the Scientific Director of the Big 10/ Ivy league Consortium on Concussion and he also serves as a member on the Scientific Advisory Boards of the US National Football League (NFL), the National Collegiate Athletic Association (NCAA)-DoD Grand Alliance, “Concussion Assessment, Research and Education” (CARE) Consortium and the International Concussion Society.
For his research efforts, Dr. Smith is Principal Investigator of several multi-center research programs on concussion and TBI-induced neurodegeneration. Dr. Smith also directs an NIH post-doctoral fellow training grant for brain injury. His group has established that damage to brain networks and specifically, diffuse axonal injury (DAI), represents key pathological process underlying concussion symptoms and that the extent of acute axonal pathology is predictive of cognitive outcome. In addition, his group has discovered mechanisms of concussion and more severe TBI that lead to progressive neurodegeneration, including chronic traumatic encephalopathy. These collective efforts are represented in over 250 published scientific reports with an h-index of over 80. -
Read More about David Meaney, PhD
David Meaney, PhD
CBIR Associate Director for Preclinical Research, Bioengineering
David Meaney, PhD
CBIR Associate Director for Preclinical Research, Bioengineering
Dr. Meaney is the S.R. Pollack Professor and Senior Associate Dean, Department of Bioengineering and has published extensively on the subject of traumatic brain injury. His research program concentrates on studying the role of mechanical forces in traumatic brain injury (TBI). Using in vitro systems to understand the mechanisms for mechanosensitive receptors and channels in the brain and outcome after TBI. Moreover, his laboratory studies how these activated pathways will influence the function of neural circuits after injury. They are now using the same design process for developing a model of primary blast TBI in the mouse.
-
Read More about Ramon Diaz-Arrastia, MD, PhD
Ramon Diaz-Arrastia, MD, PhD
Associate Director for Clinical Research, Penn Center for Brain Injury and Repair
Ramon Diaz-Arrastia, MD, PhD
Associate Director for Clinical Research, Penn Center for Brain Injury and Repair
Associate Director for Clinical Research, Penn Center for Brain Injury and Repair, Presidential Professor of Neurology, Attending Neurologist, Penn Presbyterian Medical Center Hospital of the University of Pennsylvania, Pennsylvania Hospital, Dr. Diaz-Arrastia is endowed as a University Presidential Professor (a diversity chair) and has a long history in training with an emphasis on diversity. He leads the TBI Clinical Research Initiative at the newly established Level I Trauma Center at Penn Presbyterian Medical Center. Dr. Diaz-Arrastia’s research focus is imaging and molecular biomarkers of TBI in humans. The focus of his laboratory is traumatic microvascular injury (TMI) with the goal of developing prognostic, predictive, and pharmacodynamic biomarkers of TMI, in order to efficiently design clinical trials of angioprotective and angioregenerative therapies.
CBIR Collaborators
-
-
 Rosette C. Plotkin Biester, PhDRead More about
Rosette C. Plotkin Biester, PhDRead More about
Rosette C. Plotkin Biester, PhD
Adjunct Assistant Professor, Department of Physical Medicine and Rehabilitation Director, Neuropsychology, Polytrauma Neuropsychologist, Philadelphia Veterans Affairs Medical Center, Dr. Biester's research has focused on the comprehensive assessment of neurocognitive impairments, mood disturbance, quality of life, and functional/behavioral changes associated with traumatic brain injuries, stroke, and pulmonary conditions including acute respiratory distress syndrome and pulmonary hypertension. Her extensive inpatient and outpatient clinical experience in neuropsychology has promoted clinical research in testing specific cognitive domains most susceptible to change, including working memory, auditory memory, and executive functions.
-
Read More about H. Isaac Chen, MD
H. Isaac Chen, MD
Neurosurgery
H. Isaac Chen, MD
Neurosurgery
Assistant Professor of Neurosurgery at the Presbyterian Medical Center of Philadelphia and the Veteran's Administration Medical Center Department of Neurosurgery, Dr. Chen's clinical interests include functional neurosurgery (i.e., deep brain stimulation and epilepsy surgery), the resection of tumors in and around eloquent brain tissue, and traumatic brain injury. With respect to clinical research, he works on developing new techniques for mapping brain function and identifying targets for neuro-modulatory and brain circuit reconstruction interventions.
Dr. Chen’s laboratory focus is developing novel methods for reconstructing brain circuitry after injury, specifically using structured neural tissues. This work draws from stem cell biology, neural tissue engineering, and neural interface technologies.
-
Read More about Akiva S. Cohen, PhD
Akiva S. Cohen, PhD
Associate Professor, Neurology
Akiva S. Cohen, PhD
Associate Professor, Neurology
Associate Professor, Neurology, Children’s Hospital of Philadelphia, University of Pennsylvania, Dr. Cohen focuses on defining the mechanisms that underlie cognitive impairment and a reduction in seizure threshold caused by TBI. The laboratory employs methods that span the systemic to cellular levels including hippocampal-dependent behavior, brain slices physiology, voltage sensitive dye recording as well cellular biochemistry and immunohistochemistry.
-
Diego Contreras, MD, PhDRead More about
Diego Contreras, MD, PhD
Diego Contreras, MD, PhD, Professor of Neuroscience, Department of Neuroscience, University of Pennsylvania
Dr. Contraras’ research interest focus is on how the intrinsic cellular properties of neurons and the characteristics of local neuronal networks contribute to the encoding of peripheral sensory input in two separate animal models: (i) the cat visual system and (ii) the rat whisker system. Responses to sensory stimuli are recorded from the neocortex and thalamus in vivo using intracellular and optical voltage-sensitive dye methods. These methods are also applied to the brain slice preparation in order to further study the dynamics of cortical microcircuitry.
-
D. Kacy Cullen, PhDRead More about
D. Kacy Cullen, PhD
D. Kacy Cullen, PhD, Research Assistant Professor, Department of Neurosurgery
Dr. Cullen’s research program operates at the intersection of neurotrauma and neural engineering by applying biomedical engineering principles to better understand the causative mechanisms of neural injury as well as to develop tissue engineering-based treatments to restore function. Dr. Cullen investigates injury biomechanics, biophysical responses, and pathophysiology following injury to the nervous system. His group also develops tissue-engineered strategies for biohybrid neurotechnology to mitigate trauma-induced deficits or augment the body’s capacity for regeneration.
-
John A. Detre, MDRead More about
John A. Detre, MD
John A. Detre, MD, Professor of Neurology and Radiology, Director, Center for Functional Neuroimaging
Dr. Detre's research focuses brain imaging and its applications in basic and clinical neuroscience. Much of the work involves methodological development and validations arterial spin labeled perfusion MRI as well as its use as a biomarker of brain function and its modulation by disease, pharmacological therapies or other interventions. These studies are used for examination of brain development and developmental disorders, degenerative diseases, brain tumors, and traumatic brain injury.
Center for Functional Neuroimaging at the University of Pennsylvania
-
Read More about James Eberwine, PhD
James Eberwine, PhD
Pharmacology
James Eberwine, PhD
Pharmacology
James Eberwine, PhD, Elmer Holmes Bobst Professor of Pharmacology, Co-Director of the Penn Genome Frontiers Institute
Dr. Eberwine is a molecular neurobiologist whose research efforts focus on understanding the functioning of individual neurons and subregions of neurons, called dendrites, by using molecular biological tools. He has developed various analytical procedures that permit characterization of the mRNA and protein complement of single cells.
Hospital of the University of Pennsylvania's Department of Psychiatry
-
Joshua Gold, PhDRead More about
Joshua Gold, PhD
Joshua Gold, PhD, Professor of Neuroscience, Department of Neuroscience, University of Pennsylvania
The main goal of Dr. Gold’s laboratory is to understand how the brain learns from experience to make more effective decisions. The foundation for their work is quantitative behavioral measurements, which define what is learned. They then use direct measurements of brain activity in monkeys and indirect measurements of brain activity in humans to identify these learning- dependent computations. He is particularly interested in how this brain activity is altered and then recovers after injury. Dr. Gold also directs his efforts towards advancing the outstanding training environment at Penn as Chair of the Neuroscience Graduate Group, overseeing over 100 students and 130 faculty.
-
Matthew Grady, MD, FAAP, CAQSMRead More about
Matthew Grady, MD, FAAP, CAQSM
Matthew Grady, MD, FAAP, CAQSM, is a pediatric sports medicine specialist in The Children’s Hospital of Philadelphia’s Department of Orthopedic Surgery.
Areas of Expertise: Concussions in pediatric athletes, Injury prevention, Overuse injuries in pediatric athletes, Pediatric injuries, Stress fractures
Dr. Grady is a board-certified pediatrician with a Certificate of Added Qualification (CAQ) in primary care sports medicine. He is also a Clinical Assistant Professor of Pediatrics at the University of Pennsylvania Perelman School of Medicine, where he is Director of the Primary Care Sports Medicine Fellowship program, and is responsible for training CHOP Emergency Department fellows, pediatric residents and medical students.
-
M. Sean Grady, MDRead More about
M. Sean Grady, MD
M. Sean Grady, MD, Charles Harrison Frazier Professor
Dr. Grady is an academic neurosurgeon whose basic science research interests are dedicated to TBI. Until recently, Dr. Grady had NIH support for bench research focused on the consequences of traumatic brain injury on the hippocampus. Using both rat and mouse strains he is exploring the consequences of fluid-percussion brain injury using anatomic, electrophysiologic, and molecular techniques. These efforts are complemented by cell death analysis using the stereologic technique of optical fractionation.
-
Roy Hamilton, MD, MSRead More about
Roy Hamilton, MD, MS
Roy Hamilton, MD, MS, Assistant Professor, Departments of Neurology and Physical Medicine and Rehabilitation and the Director of the Laboratory for Cognition and Neural Stimulation, and Assistant Dean of Diversity and Inclusion at the Perelman School of Medicine at the University of Pennsylvania
The central thrust of Dr. Humilton’s research is to use noninvasive electrical and magnetic brain stimulation to explore the characteristics and limits of functional plasticity in the intact and injured human brain. Using a multidisciplinary approach that combines brain stimulation, behavioral measures, and neuroimaging, Dr. Hamilton has explored a variety of topics, including plastic changes that occur in the brains of blind individuals, mechanisms of neural recovery in patients who have suffered from strokes, and neuromodulation as a potential tool for remediating disorders of cognition.
Dr. Hamilton's Laboratory for Cognition and Neural Stimulation
-
Frances Elizabeth Jensen, MD, FACPRead More about
Frances Elizabeth Jensen, MD, FACP
Frances Elizabeth Jensen, MD, FACP, Professor of Neurology, CPUP Board of Directors, University of Pennsylvania, Chair, Neurology Department
The primary focus of Dr. Jensen’s research is to investigate pathophysiological mechanisms of epilepsy, including post-traumatic, and secondary effects on synaptic plasticity. A secondary goal is to elucidate age-dependent differences in such mechanisms, and to examine the interactions between brain development, excitotoxic brain injury, epilepsy and cognition. Neurotransmitter receptors are developmentally regulated, and we have specifically demonstrated critical roles of these receptors, as well as their upstream modulators and downstream effectors, in neuronal and glial cells that are unique to the immature, implying age-specific disease mechanisms.
-
Victoria E. Johnson, MBChB, PhDRead More about
Victoria E. Johnson, MBChB, PhD
Dr. Johnson received both her medical degree and PhD from the University of Glasgow, UK. She then pursued a post-doctoral fellowship with Dr. Douglas H. Smith, M.D. at the Dept. Neurosurgery, University of Pennsylvania and the Penn Center for Brain Injury and Repair.
Her research focuses on the chronic neuropathological sequelae of traumatic brain injury (TBI), including the links between TBI and neurodegenerative disease. Specifically, Dr Johnson has extensive experience in examining post—mortem brain tissue acutely and chronically following TBI in humans. In recent publications, Dr. Johnson and colleagues demonstrated that even a single TBI is associated with an increased incidence of Alzheimer-associated pathologies many years after injury. Moreover, it was identified that a single severe TBI can also induce chronic neuroinflammation, axonal pathology and blood brain barrier (BBB) permeability that can persist for months and even years in some individuals after injury. More recent work endeavors to better understand the specific mechanisms of BBB dysfunction both acutely and chronically post-TBI.
Understanding the temporal changes following TBI by examining both clinical material and utilizing novel model systems, will be critical for the development of treatments for TBI patients. -
Kelly Jordan-Sciutto, PhDRead More about
Kelly Jordan-Sciutto, PhD
Kelly Jordan-Sciutto, PhD, Chair and Professor, Department of Pathology, Associate Dean for Graduate Education and Director of the Biomedical Graduate Studies at the Perelman School of Medicine, University of Pennsylvania
Dr. Jordan-Sciutto’s laboratory investigates mechanisms that underly neuronal damage and death in response to neuroinflammatory stimuli including HIV-associated neurocognitive disorder, Alzheimer disease, Parkinson Disease, and trauma. She is particularly interested in molecular signaling pathways including the endogenous antioxidant response, the unfolded protein response, cell death pathways and cell cycle progression. She uses genetic, cellular, molecular, and behavioral approaches and uses both in vitro and in vivo models.
-
Michael Kahana, PhDRead More about
Michael Kahana, PhD
Michael Kahana, PhD, Professor of Psychology, Department of Psychology, University of Pennsylvania
Dr. Kahana’s Research interests include computational modeling and experimental studies of human learning and memory. Much of the research has focused on using sophisticated measures of episodic memory to develop a detailed understanding of how various types of associations influence recall. Together with colleagues, Kahana has developed context-based mathematical models of human episodic memory to account for these data. Additional experimental work has been focused on the electrophysiological correlates of cognitive processes, including recoding of local-field potentials and single neuron activity in humans.
-
Todd Kilbaugh, MDRead More about
Todd Kilbaugh, MD
Todd Kilbaugh, MD, Anesthesiologist and Pediatric Intensivist Department of Anesthesiology and Critical Care The Children's Hospital of Philadelphia University of Pennsylvania
Dr. Kilbaugh’s research focus is in mitochodrial dysfunction following traumatic brain injury in preclinical models as well as in clinical studies.
-
Virginia Man-Yee Lee, PhDRead More about
Virginia Man-Yee Lee, PhD
Virginia Man-Yee Lee, PhD, Professor of Pathology and Laboratory Medicine, Co-Director of the Center for Neurodegenerative Disease Research at Perelman School of Medicine, University of Pennsylvania
Dr. Lee’s research focuses on the etiology and pathogenesis of alpha-synuclein, tau, TDP-43, and other misfolded disease proteins in the pathobiology of neurodegenerative diseases and injury, including Alzheimer's disease, Parkinson's disease, frontotemporal dementias, amyotrophic lateral sclerosis and TBI (including TBI-induced Alzheimer’s disease and chronic traumatic encephalopathy). A multidisciplinary approach, that includes biochemical and molecular studies of neuronal culture systems, animal models and human tissues obtained at autopsy, is used in the laboratory to address these research issues in common with these neurodegenerative diseases and how they are linked with brain injury.
University of Pennsylvania's Department of Pathology and Laboratory Medicine
$3 Million Breakthrough Prize in Life Sciences for Virginia Lee
-
Joshua Levine, MDRead More about
Joshua Levine, MD
Joshua Levine, MD, Assistant Professor, Departments of Neurology, Neurosurgery, Anesthesiology & Critical Care, Director, Neurocritical Care Program, Hospital of the University of Pennsylvania, Director, Neurocritical Care Fellowship Training Program, Hospital of the University of Pennsylvania
Dr. Levine specializes in the care of patients with severe injury to the nervous system, including patients with acute traumatic brain and spine injury, those with subarachnoid hemorrhage, ischemic stokes, intracerebral hemorrhages, acute seizures, brain infections, and severe acute neuromuscular disorders. His research interests include defining the optimal use of advanced technology to monitor the brain for secondary injury, and the role of inflammation and coagulation in the pathogenesis of delayed ischemic injury after subarachnoid hemorrhage.
-
Christina Master, MD, FAAP, CAQSMRead More about
Christina Master, MD, FAAP, CAQSM
Christina Master, MD, FAAP, CAQSM, Division of Orthopedics and Sports Medicine, The Children’s Hospital of PhiladelphiaChildren's Hospital of Philadelphia
Dr. Master is Associate Professor of Clinical Pediatrics at the University of Pennsylvania Perelman School of Medicine and Associate Program Director of the Primary Care Sports Medicine fellowship at CHOP with over two decades of experience in clinical pediatrics. Dr. Master is board-certified in pediatrics and brain injury medicine with additional qualification in sports medicine and treats over a thousand youth with concussion annually in her outpatient practice. She is co-founding director of Minds Matter, the concussion program for children at CHOP that provides clinical care, community outreach and conducts research in youth concussion. Her particular research emphasis has been describing the epidemiology of pediatric concussion and identifying vestibular and visual deficits following concussion as a target for intervention for those with prolonged symptoms.
-
Michael L. McGarvey, MDRead More about
Michael L. McGarvey, MD
Michael L. McGarvey, MD, Associate Professor of Neurology at the Hospital of the University of Pennsylvania Director Intraoperative Monitoring, Hospital of the University of Pennsylvania
As Director of the Intraoperative Monitoring Program at the University of Pennsylvania, Dr. McGarvey performs complex neurophysiologic testing during surgical procedures including EEG, evoked potentials, and EMG. He has completed post-residency training in Stroke and Intraoperative monitoring and is an active member in the American Stroke Association and American Neurophysiology Society. Dr. McGarvey's research efforts include intraoperative neuroprotection, neurophysiologic monitoring techniques and identification of biologic markers of neurologic injury.
-
Claire Mitchell, PhDRead More about
Claire Mitchell, PhD
Claire Mitchell, PhD, Associate Professor, Department of Anatomy and Cell Biology, University of Pennsylvania
Dr. Mitchell’s current research interests focus on linking mechanical strain with inflammatory responses in the retina. Acute and chronic elevations in pressure lead to the mechanosensitive release of ATP through pannexin hemichannels, with subsequent autostimulation of P2X7 receptors. Moderate stimulation of these P2X7 receptors on astrocytes can prime expression of the NLRP3 inflammasome and other cytokines, activate the inflammasome and trigger cytokine release. More pronounced stimulation of the P2X7 receptor on retinal ganglion cells can lead to cell death. This provides a powerful model to explain inflammation and death with TBI, and identifies several key points of intervention.
-
Nicole Otto, MDRead More about
Nicole Otto, MD
Nicole Otto, MD, Clinical Assistant Professor of Family Medicine and Community Health Staff Physician, University of Pennsylvania Student Health Services
Through Dr. Otto’s Student Health practice, she specializes in the care of the young adult (ages 17-35, primarily), including diagnosis and treatment of acute illness and injuries, as well as management of chronic disease such as mental health conditions, eating disorders, cardiovascular, and endocrine conditions.
-
Jose L. Pascual, M.D., Ph.D. FRCS(C), FRCP(C)Read More about
Jose L. Pascual, M.D., Ph.D. FRCS(C), FRCP(C)
Jose L. Pascual, M.D., Ph.D. FRCS(C), FRCP(C), Assistant Professor, Surgery, University of Pennsylvania
Dr. Pascual is certified in Surgical and Neurocritical Care as well as Trauma and General Surgery. He is co-medical director of the Surgical Intensive Care Unit at the Hospital of the University of Pennsylvania (HUP). His clinical and research interests are in shock and head injury. His research work is shared in clinical and basic science to learn how a variety of insults including head injury and shock affect the microcirculation and how different management strategies influence their effects. This basic science work is translated into several clinical projects both retrospective and prospective evaluating the effects of different therapeutic agents in traumatic brain injured patients as well as the immunemodulating effects of different resuscitation fluids in different forms of shock.
-
Danielle Sandsmark, MD, PhDRead More about
Danielle Sandsmark, MD, PhD
Danielle Sandsmark, MD, PhD, Assistant Professor of Neurology at the Hospital of the University of Pennsylvania
Dr. Sandsmark is a neurologist who focuses on the care of patients with severe brain injuries treated in the neurological intensive care unit. Her research interest is in long-term clinical outcomes after severe traumatic brain injury. She is interested in understanding and developing clinical markers that can be detected at the time of injury and are predictive of long-term cognitive and functional outcomes after traumatic brain injury. She works in collaboration with colleagues in neurosurgery, physical medicine and rehabilitation, and neuropsychology to better understand how individuals recover after moderate-severe traumatic brain injury.
-
Andrea L.C. Schneider, MD, PhDRead More about
Andrea L.C. Schneider, MD, PhD
Andrea L.C. Schneider, MD, PhD, Assistant Professor of Neurology, Division of Neurocritical Care, University of Pennsylvania
Dr. Schneider received her MD in 2014 from the Johns Hopkins University School of Medicine and received her PhD in Epidemiology from the Johns Hopkins University Bloomberg School of Public Health in 2012. She completed Neurology Residency and Neurocritical Care Fellowship at the Johns Hopkins Hospital in 2020. Her research is focused on how pre-existing vascular risk factors and vascular injury in traumatic brain injury impact recovery, especially cognitive recovery, after traumatic brain injury.
-
Vivek Shenoy, PhDRead More about
Vivek Shenoy, PhD
Vivek Shenoy, PhD, Professor of Materials Science and Engineering (MSE), Mechanical Engineering and Applied Mechanics (MEAM), Bioengineering (BE)
Dr. Shenoy's current research focuses on developing theoretical concepts and numerical methods to understand the basic principles that control the behavior of both engineering and biological systems. A significant challenge in modeling the engineering and biological systems we study is that important processes involve coupling of both small-scale (atomic or single molecule) phenomena and long-range (elastic, electromagnetic) interactions over length scales of hundreds of nanometers. The goal of his group's work is to address these issues by combining atomic scale simulation methods with continuum or mesoscale theories and by adapting insights from condensed matter physics, solid mechanics, chemistry, materials science and applied mathematics.
-
Randel Swanson, DO, PhDRead More about
Randel Swanson, DO, PhD
Randel Swanson, DO, PhD, Assistant Professor of Physical Medicine and Rehabilitation at the Hospital of the University of Pennsylvania
Dr. Swanson provides comprehensive Neurological Rehabilitation Care to patients with Acquired Brain Injury, in both the inpatient and outpatient setting. His goal is to assist patients in achieving optimal return of neurological function following all forms of Brain Injury, including Traumatic Brain Injury (TBI), Concussion, Anoxic Brain Injury, Cerebral Vascular Accidents (CVA or Stroke), Brain Tumors, Movement Disorders and Neurodegenerative Disorders. In managing secondary complications from Acquired Brain Injury, Dr. Swanson performs chemodenervation (Botulinum toxin, Phenol or Alcohol) techniques for the treatment of spasticity and dystonia.
-
Ragini Verma, PhDRead More about
Ragini Verma, PhD
Ragini Verma, PhD, Associate Professor Biomedical Image Analysis, Department of Radiology at the University of Pennsylvania
Dr. Verma focuses on biomedical image analysis with the Department of Radiology at the University of Pennsylvania. Dr. Ragini is an expert in diffusion image analysis and has extensive experience developing mathematically intensive computationally efficient tools for addressing several challenging aspects of diffusion-based computationally neuroanatomy, such as, registration, population-based statistical analysis and multi-parametric analysis of high dimensional data using pattern classification techniques. Her research focus encompasses diffusion imaging, multi-modal connectiomics, and genetic underpinnings of the brain’s network structure and how the network changes with the injury.
-
William C. Welch, PhDRead More about
William C. Welch, PhD
William C. Welch, PhD, Chair, Department of Neurosurgery, Pennsylvania Hospital
Dr. Welch is the Co-Director of the Neurosurgical Biomechanical Research Laboratory and oversees research related primarily to biomechanical assessments of the treated and untreated spine. His clinical activities and clinical trials revolve around spinal disorders and motion preservation. He was honorably discharged as a Lieutenant Commander from the United Stated Naval Reserves in 1998 after ten years of service.
-
Tamara L. Wexler, MD, PhDRead More about
Tamara L. Wexler, MD, PhD
Tamara L. Wexler, MD, PhD, Adjunct Assistant Professor, Endocrinology, Diabetes and Metabolism
Dr. Wexler is an endocrinologist specializing in neuroendocrinology and reproductive endocrinology. She has served as an Attending Physician in Internal Medicine at the Massachusetts General Hospital and as the Director of the NYU Langone Medical Center Pituitary Center, where she built the infrastructure to facilitate clinical research. She has established national inter-institute and multidisciplinary collaborations to investigate the role of neuroendocrine dysfunction after brain injury, and is an internationally recognized expert in post-TBI pituitary dysfunction, speaking at global conferences and writing for both the lay and professional audience.
Dr. Wexler received her medical degree and PhD in Neuroscience from the University of Pennsylvania, conducting dissertation research into the pathophysiology of Kallmann’s Syndrome at the University of Pennsylvania and the National Institutes of Health. She completed her residency in Internal Medicine and fellowship in Endocrinology, Diabetes, and Metabolism at the Massachusetts General Hospital, where she was part of the multidisciplinary Neuroendocrine Unit, designed and ran national clinical trials on the impact of growth hormone, and served for 12 years on the MGH Optimum Care Committee.
While remaining on staff at the Massachusetts General Hospital, Dr. Wexler spent four years at McKinsey & Company, where she served as the Global Lead for Endocrinology. She reviews grants for the Bill and Melinda Gates Foundation in the area of reproductive health; is an invited member of the University of Pennsylvania Institute for Diabetes, Obesity, and Metabolism Leadership Council; consults as an expert on research and development programs; and serves on the editorial board of Endocrine Today and the Endocrine Society-Medscape Consults program. She is an active member of The Endocrine Society, for which she served on the Advocacy and Public Outreach core committee, and was recently elected to the Scientific and Educational Programs Core Committee. She is a speaker and moderator at academic medical centers and national conferences on the topic of pituitary function and post-TBI endocrine disorders. Her publications appear in the Journal of Clinical Endocrinology & Metabolism and Clinical Endocrinology, among other journals.
https://med.nyu.edu/faculty/tamara-wexler
https://neuroendocrineassociates.com/about
-
Beth Winkelstein, PhDRead More about
Beth Winkelstein, PhD
Beth Winkelstein, PhD, Vice Provost for Education and Professor, Bioengineering
The broad goal of Winkelstein’s research is to understand the mechanisms of injury from sports, automotive and degenerative conditions, especially those injuries that produce pain. By combining biomechanical and immunological techniques, her lab can define the relationships between injury to the cervical spine/neck and physiological cascades of persistent pain. Particular emphasis is placed on understanding injury to individual structures in the neck, such as the facet joints, nerve roots and spinal cord and how mechanical loading to these structures elicits pain. Through this work she can begin to develop thresholds for mechanical injury that produce persistent pain; and work towards a definition of the neck’s tolerance for painful injury. Additional research efforts are aimed at understanding the role of biomechanics in the neuroimmunologic changes of the central nervous system that contribute to persistent pain.
University of Pennsylvania's Department of Bioengineering
Spine Pain Research Lab -
Read More about Alexandra V. Ulyanova, PhD
Alexandra V. Ulyanova, PhD
Assistant Professor of Neurosurgery
Alexandra V. Ulyanova, PhD
Assistant Professor of Neurosurgery
Dr. Ulyanova’s goals are to understand the role sleep and circadian rhythm abnormalities in the development of post-traumatic epileptogenesis and their contribution to the cognitive deficits observed following traumatic brain injury. Dr. Ulyanova research is focused on integration of large-scale electrophysiology with cognitive behavioral outcomes to understand network interactions within and between deep brain structures.
-
John A. Wolf, PhDRead More about
John A. Wolf, PhD
John A. Wolf, PhD, Assistant Professor of Neurosurgery at the Hospital at the University of Pennsylvania
Dr. Wolf’s research program is highly collaborative, and focuses on a number of broad areas related to neurotrauma and repair. Trained as a computational and systems level neuroscientist, Dr. Wolf’s goals are a deeper understanding of the role of diffuse brain injury in disrupting communication between and within brain regions. Dr. Wolf is also leading electrophysiological efforts to integrate electrodes with nervous tissue in vitro so that it can then be implanted for both peripheral and central nervous system repair.
-
John H. Wolfe, PhDRead More about
John H. Wolfe, PhD
John H. Wolfe, PhD, Professor of Neurology, Children's Hospital of Philadelphia
Dr. Wolfe's research interests include somatic cell gene transfer to the brain. Animal homologues of human neurodegenerative genetic diseases are used as test systems for gene transfer by viral and other vectors. Ex vivo gene transfer is being studied using retrovirus vector-corrected cells, which are transplanted directly into the brain to circumvent the blood-brain barrier. Multipotent neural progenitor cells, which differentiate into mature normal cells appropriate to their location within the brain, are being evaluated for their ability to deliver engineered cells to many regions of the diseased brain.