Updated data
Funded by the Laura and John Arnold Foundation, we collaborated with the Bridgespan Group and ORGANIZE from May 2016-May 2017 to build upon the HRSA-sponsored Deceased Donor Potential Study to provide a more accurate estimate of the deceased donor potential in the US, while also proposing potential metrics of organ procurement organization (OPO) performance that could be operationalized using these administrative data. This work utilized data from the Nationwide Inpatient Sample (NIS) from 2009-2012 and data from State Inpatient Databases (SIDs) from 25 states during this same period. This work was published in the American Journal of Transplantation in 2017 (https://onlinelibrary.wiley.com/doi/epdf/10.1111/ajt.14391), with updated data published in Transplantation in 2018 (file:///C:/Users/dago/Downloads/Important_Facts_About_Organ_Donation_and_OPO.39%20(1).pdf).(1,2) Although these analyses were rooted in the HRSA-sponsored and UNOS-led Deceased Donor Potential Study, several refinements were made: a) additional codes to exclude patients with severe sepsis; b) categorization of potential donors as a potential donation after neurologic determination of death (DNDD) vs donation after circulatory determination of death (DCDD) donor based on published estimates (3-6); c) exclusions of older potential donors who would have been classified as a potential DCDD donor; and d) organ-specific estimates based on expected organ yield per donor.
Through a partnership with the Agency for Healthcare Research and Quality (AHRQ), we were able to update the results of our study by leveraging data from the SIDs of 45/50 states, comprising 49/58 of the donor service areas (DSAs; geographic area covered by a respective organ procurement organization [OPO]). The method to identify a ‘possible’ deceased donor, based on prior published work (7,8,9) and validated against medical records data from two OPOs1, was to use administrative data to identify in-hospital deaths among patients: 1) ≤75 years of age; 2) ventilated; 3) absence of multi-organ system failure, severe sepsis, cancers contraindicating donation; 4) died from a cause consistent with organ donation, with an in-hospital length of stay ≤14 days.
What is evident is that at 50% donation rates, there could have been nearly 6,000 more lifesaving organ transplants per year between 2012 and 2014, and with 100% donation rates, more than 25,000 additional lifesaving organ transplants could have been performed each year in the US.
More specifically, based on these data:
- With 50% donation rates (Figure 1), there could have been:
- >3,700 more kidney transplants/year
- >1,700 more liver transplants/year
- >300 more lung transplants/year
 >300 more heart transplants/year
>300 more heart transplants/year
- With 100% donation rates (Figure 2), there could have been:
- >17,000 more kidney transplants/year
- >7,500 more liver transplants/year
- >1,400 more lung transplants/year
- >1,400 more heart transplants/year
Additionally, these updated data have also yielded several other key findings:
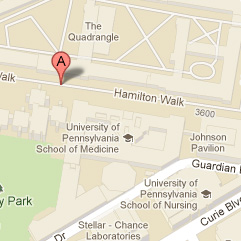
- Marked variability in organ donation rates across the US (Figure 3). Data from the SIDs, which included hospital zip codes, allowed us to map the inpatient deaths to DSA to estimate the donor potential within a DSA (the total donor potential for a given OPO). The donation rate was calculated as: (number of organ donors) / (‘possible’ deceased donors), with possible donors based on the methodology described above. As shown to the right, there was marked variability in organ donation rates, without geographic clustering, with areas of high donation (e.g., San Diego and Philadelphia) adjacent to areas of low donation (Los Angeles and New York).
- The unrealized number of donors across the US relates both to local organ donation rates and the underlying population (Figure 4). The unrealized donor potential in terms of absolute numbers is attributable to the variability in organ donation rates, but is further magnified in areas with a large underlying population. As shown to the right, the greatest potential for increasing the number of organ donors is in California (Los Angeles and San Francisco OPOs) and New York. Figure 1b demonstrates that if the donation rates in these three DSAs were at the level of the 90th percentile DSA (whose donation rate is approximately 50%), then >500 additional deceased donors could have been realized in those three areas.
References
1. Goldberg D, Kallan MJ, Fu L, et al. Changing Metrics of Organ Procurement Organization Performance in Order to Increase Organ Donation Rates in the United States. American Journal of Transplantation 2017;17(12):3183-3192.
2. Goldberg DS, Shafer T, Siminoff L. Important Facts About Organ Donation and OPO Performance. Transplantation 2018;102(5):e249-e250.
3. Gore SM, Taylor RM, Wallwork J. Availability of transplantable organs from brain stem dead donors in intensive care units. BMJ 1991;302(6769):149-153.
4. Schnuriger B, Inaba K, Branco BC, et al. Organ donation: an important outcome after resuscitative thoracotomy. Journal of the American College of Surgeons 2010;211(4):450-455.
5. Earl-Royal E, Kaufman EJ, Hsu JY, Wiebe DJ, Reilly PM, Holena DN. Age and preexisting conditions as risk factors for severe adverse events and failure to rescue after injury. The Journal of Surgical Research 2016;205(2):368-377.
6. Scalea JR, Redfield RR, Rizzari MD, et al. When Do DCD Donors Die?: Outcomes and Implications of DCD at a High-volume, Single-center OPO in the United States. Annals of Surgery 2016;263(2):211-216.
7. Holt AW, Hodgeman GK, Vedig AE, Heard PE. Organ donor index: a benchmark for comparing hospital organ donor rates. The Medical Journal of Australia 1999;170(10):479-481.
8. Rose C, Nickerson P, Delmonico F, Randhawa G, Gill J, Gill JS. Estimation of Potential Deceased Organ Donors in Canada. Transplantation. 2016;100(7):1558-1563. 9. Klassen DK, Edwards LB, Stewart DE, Glazier AK, Orlowski JP, Berg CL. The OPTN Deceased Donor Potential Study: Implications for Policy and Practice. American Journal of Transplantation 2016;16(6):1707-1714.