Adolescent Nutrition and Malnutrition
Key Conditions
- Anorexia nervosa
- Bulimia nervosa
- Overweight and Obesity
- Refeeding syndrome
- Where to find in the PSOM curriculum
- General Information
- Clinical Approach
- History
- Key Physical Exam
- Differential Diagnosis
- Evaluation and Management
- Pearls
- Resources/References
- Knowledge Check #1
- Teacher's Corner
- Core 1 (Pre-Clerkship)
- Brain and behavior – Eating disorders
- Gastroenterology – Nutrition and obesity
- Core 2 (Clerkship)
- Pediatric Clerkship - Growth and Nutrition Didactic
- Related; Family Medicine - Didactics on T2DM, HTN (DASH diet), General Surgery - Problem-based learning on TPN, Neurology - Vitamin deficiencies and their neurological consequences
- Core 3 (Post-Clerkship)
- Nutrition during adolescence is crucial due to the significant ongoing growth and maturation that occurs during this period. Sociobehavioral factors can highly influence nutrition during this period as adolescents are exploring independence and are prone to model behavior after peer influences. As such adolescents are prone to fad diets many of which can lead to nutrient deficiencies.
- Many adolescents in the US do not consume sufficient amounts of minerals, vitamins, and nutrients, including folic acid, vitamins A, D, E, and B6, calcium, iron, zinc, magnesium, and fiber.
- Adolescence is a very important time for bone mass development with 40-60% of adult bone mass accrued during adolescence (AAP Pediatric Nutrition).
- Undernutrition in adolescence is commonly caused by eating disorder or psychiatric disorders such as depression
- Anorexia nervosa – DSM-5 diagnosis that requires 1) restriction of energy intake that leads to low body weight 2) intense fear of gaining weight, 3) Distorted perception of body weight and shape, undue influence of body weight or shape on self-worth, lack of recognition of seriousness of low body weight
- Types: Restricting and binge-eating/purging
- Bulimia nervosa – DSM-5 diagnosis that includes 1) recurrent episodes of binge eating; 2) recurrent inappropriate compensatory behaviors (i.e. self-induced vomiting, misuse of laxatives, diuretics, excessive exercise); 3) both binge eating and compensatory behaviors occur at least 1x/week for at least 3 months; 4) self-evaluation is unduly influenced by body shape and weight; 5) Does not occur during episodes of anorexia nervosa
- Anorexia nervosa – DSM-5 diagnosis that requires 1) restriction of energy intake that leads to low body weight 2) intense fear of gaining weight, 3) Distorted perception of body weight and shape, undue influence of body weight or shape on self-worth, lack of recognition of seriousness of low body weight
- Overnutrition is also a form of malnutrition arising from excessive intake of nutrients, resulting in overweight or obesity
- Overweight - BMI ≥85th and <95th percentile for age and sex
- Obesity - BMI ≥95th percentile for age/sex
- Patients should be screened for dyslipidemia, hypertension, type 2 diabetes, metabolic dysfunction-associated steatotic liver disease (MASLD)
- Binge eating disorder – DSM-5 eating disorder diagnosis characterized by episodes of binge eating marked by lack of control and distress regarding behaviors
- More common in individuals with obesity but can occur at normal weights
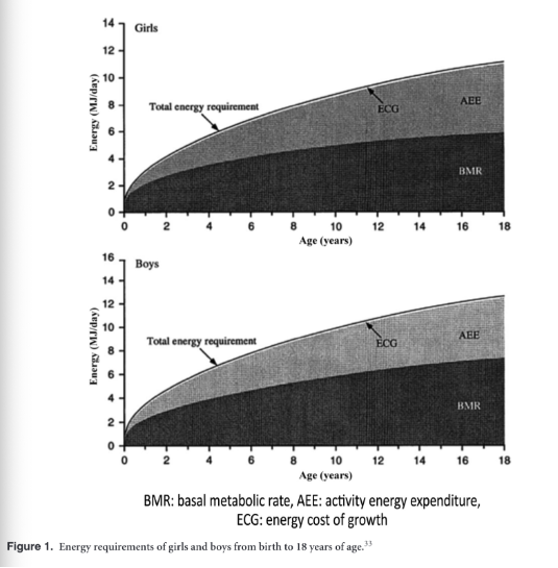
(Das et et al., 2017)
Clinical Vignette: A 15 yo M presents to clinic with his parents who are concerned by his recent weight loss. At his last well child visit at age fourteen, he was noted to be above the 95%ile BMI and he was recommended to increase his physical activity and decrease processed foods. At today's visit, it is noted that he has lost 40 lbs in the past year and now has a BMI of 16 or in the 4%tile. While talking with the doctor alone, he mentions that he has been bullied at school for his weight which is why he started losing weight. Now, he reports eating only one meal per day of “clean” foods because he is afraid to become “fat” again. He recognizes that his parents have been worried about his weight gain but he is still worried about his “flabby” midsection. He has no episodes of binging food, intentional vomiting, excessive exercise, or laxative use.
Objectives
- Identify clinical features and red flags in adolescents that suggest an eating disorder
- Outline the key components of the history, physical exam, and initial laboratory evaluation for adolescents presenting with significant weight loss and potential malnutrition
- Recognize the risks and management principles of refeeding syndrome in malnourished adolescents
Key features to explore for adolescent history when concerned about malnutrition: (Tang et al., 2021)
- Food allergy or intolerance, any foods that are avoided?
- Dietary recall for last 24 hours
- Adequacy of access to food
- Desire to lose or gain weight
- Menstrual history in those who menstruate
- Satisfaction/dissatisfaction with body
- Parental heights
- Prior growth trajectory
- Any behaviors of purging, bingeing, use of diet pills, laxatives
- Amount of exercise
Review of systems
- Appetite changes, feeling cold/hot, sleep, mood, bowel movements, urinary changes, energy/fatigue, skin changes
- Vital signs – evaluate for orthostatic instability – orthostatic tachycardia or hypotension, bradycardia, and hypothermia
- BMI
- Mouth – look for erosion of dental enamel, hypertrophy of parotid glands (indicative of purging behaviors)
- Skin – dry skin, lanugo; skin calluses on hands (Russell’s sign)
Consider our “buckets” for undernutrition
- Inadequate energy (caloric) intake or “not enough in”
- Eating disorder with caloric restriction
- Psychiatric diagnosis – depression, psychosis
- Inadequate absorption or “too much out”
- GI pathology – Celiac, IBD
- Excessive energy expenditure due to underlying health conditions or “burning up too much”
- Endocrine –thyroid disease, Addison’s disease
- Infection – HIV, tuberculosis
- Oncology
- Rheumatologic
- When the patient had elevated BMI meeting criteria for obesity, what laboratory evaluation should have been considered?
- Lipid screening, liver function tests, diabetes evaluation
- Does this patient meet criteria for eating disorder?
- Yes, the patient meets criteria for anorexia nervosa.
- For this patient with weight loss and concern for malnutrition, what laboratory evaluation and other should be considered?
- CBC w/ differential → anemia, immunodeficiency, malignancy
- Iron studies → iron deficiency is common in children with poor growth
- Inflammatory markers and TSH to evaluate for organic causes of weight loss
- Chemistry panel → evaluate for renal tubular acidosis or metabolic alkalosis from vomiting
- Celiac disease evaluation (total IgA and tissue transglutaminase IgA) Urine analysis (infection, glycosuria, renal pathology)
- Stool studies for malabsorption or infection based on history and symptoms
- Consider HIV testing
- Consider micronutrient testing if indicated based on history and symptoms
- Orthostatic vitals measurement
- EKG for arrhythmias
- (Tang et al., 2021)
- Once the patient starts increasing caloric intake, what labs should be monitored?
- Chemistry panel should be monitored to evaluate for refeeding syndrome, which is a clinical complication resulting from fluid and electrolyte shifts that occur during nutritional rehabilitation.
- Electrolyte disturbances, such as hypophosphatemia and hypokalemia, can result in myocardial dysfunction, respiratory failure, rhabdomyolysis, and seizures.
- Weight loss in adolescents, even when beginning from an overweight status, should raise concern for eating disorders, especially when paired with distorted body image and restrictive eating behaviors.
- Refeeding syndrome is a potentially life-threatening complication of nutritional rehabilitation in malnourished adolescents, requiring careful electrolyte monitoring—particularly of phosphorus, potassium, and magnesium—when reintroducing calories.
Article
- Andrewski, E., Cheng, K., & Vanderpool, C. (2022). Nutritional Deficiencies in Vegetarian, Gluten-Free, and Ketogenic Diets. Pediatrics In Review, 43(2), 61–70. https://doi.org/10.1542/pir.2020-004275
- Das, J. K., Salam, R. A., Thornburg, K. L., Prentice, A. M., Campisi, S., Lassi, Z. S., Koletzko, B., & Bhutta, Z. A. (2017). Nutrition in adolescents: Physiology, metabolism, and nutritional needs. Annals of the New York Academy of Sciences, 1393(1), 21–33. https://doi.org/10.1111/nyas.13330
- Fisher, M. (2006). Treatment of Eating Disorders in Children, Adolescents, and Young Adults. Pediatrics In Review, 27(1), 5–16. https://doi.org/10.1542/pir.27-1-5
- Mehta, N. M., Corkins, M. R., Lyman, B., Malone, A., Goday, P. S., Carney, L. (Nieman), Monczka, J. L., Plogsted, S. W., Schwenk, W. F., & the American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Board of Directors. (2013). Defining Pediatric Malnutrition: A Paradigm Shift Toward Etiology‐Related Definitions. Journal of Parenteral and Enteral Nutrition, 37(4), 460–481. https://doi.org/10.1177/0148607113479972
- Tang, M. N., Adolphe, S., Rogers, S. R., & Frank, D. A. (2021). Failure to Thrive or Growth Faltering: Medical, Developmental/Behavioral, Nutritional, and Social Dimensions. Pediatrics In Review, 42(11), 590–603. https://doi.org/10.1542/pir.2020-001883
Books
- American Academy of Pediatrics. (2025). Pediatric Nutrition (F. R. Greer & S. A. Abrams, Eds.; 9th ed.). American Academy of Pediatrics. Itasca, IL. https://doi.org/10.1542/9781610027700
Podcast
- The Cribsiders: #59: Weight Weight…Don’t Tell Me! Countering Weight-Stigma While Providing Evidence-Based Nutrition and Preventative Health Counseling. https://thecurbsiders.com/cribsiders-podcast/59
- Podcast episode on Adolescent history taking: Adolescent Medicine | PedsCases
- Approach to Eating Disorders: Approach to Eating Disorders | PedsCases
- Obesity: Pediatric Obesity | PedsCases
- Pubertal development: pubertal-development-pir.pdf
- Eating disorders: dx-and-mx-eating-disorders-aap.pdf
Pathways
- Malnutrition, Weight Loss and Eating Disorders Clinical Pathway — ICU and Inpatient | Children's Hospital of Philadelphia
- BMI-based Evaluation and Management in Children Clinical Pathway — Outpatient Specialty Care and Primary Care | Children's Hospital of Philadelphia
Click the drop down to reveal the correct answers
Q1: A 13-year-old girl is seen for her annual well-child check. Her BMI is at the 96th percentile. She reports no significant concerns. On exam, you note mild acanthosis nigricans.
Which of the following is the most appropriate next step in evaluating this patient?
A. Serum vitamin B12 and folate
B. EKG and chest X-ray
C. Lipid panel, fasting glucose, and liver function tests
D. Bone age X-ray
Q2: A 16-year-old female with a BMI of 15 is hospitalized for nutritional rehabilitation due to anorexia nervosa. On hospital day 3, after initiation of nutritional support at 50% of goal calories, she develops generalized weakness, peripheral edema, and shortness of breath. Her labs show:
- Phosphate: 1.1 mg/dL (low)
- Potassium: 2.8 mmol/L (low)
- Magnesium: 1.3 mg/dL (low)
- Glucose: 112 mg/dL (normal)
- EKG: sinus tachycardia with QTc prolongation
Which of the following best explains the underlying pathophysiology of her clinical deterioration?
A. Volume overload due to hypoalbuminemia
B. Cellular uptake of electrolytes driven by insulin secretion
C. Increased renal losses of electrolytes from vomiting
D. Hypocalcemia from vitamin D deficiency
Q3: 17-year-old female presents to clinic for evaluation of irregular periods and fatigue. Her BMI is 16.5 kg/m². She admits to intense concern about gaining weight and restricts her intake to fewer than 800 calories per day. When asked further, she reports frequent episodes of eating large quantities of food “when she loses control,” followed by self-induced vomiting and use of laxatives to “undo the damage.” On physical exam, she is bradycardic and has dental enamel erosion and calluses on the dorsal aspects of her hands.
Which of the following is the most likely diagnosis?
A. Bulimia nervosa
B. Binge-eating disorder
C. Anorexia nervosa, binge-eating/purging type
D. Avoidant/restrictive food intake disorder (ARFID)
Answers:
Q1: C. Lipid panel, fasting glucose, and liver function tests
Rationale: Obesity (BMI ≥95th percentile) in adolescents warrants metabolic screening for diabetes, dyslipidemia, and MASLD. Acanthosis nigricans is a marker of insulin resistance.
Q2: B. Cellular uptake of electrolytes driven by insulin secretion
Rationale: In refeeding syndrome, reintroduction of carbohydrates stimulates insulin and overall anabolic state, which drives glucose and electrolytes (especially phosphate, potassium, magnesium) into cells. This leads to dangerous electrolyte shifts, causing cardiac and neuromuscular complications.
Q3: C. Anorexia nervosa, binge-eating/purging type
Rationale: The patient meets criteria for anorexia nervosa (restricting with low BMI, fear of gaining weight, and distorted body image) along with recurrent episodes of binge eating and compensatory purging behaviors, classifying her as the binge-eating/purging subtype.
PedsCases - A Learning Module for Adolescent Medicine for Medical Students | MedEdPORTAL (Cases with questions for anorexia and patient with concomitant type 1 diabetes and bulimia)
PedsCases - A Learning Module for the Approach to Childhood Obesity | MedEdPORTAL

