Appendicitis
- Where to Find in the PSOM Curriculum
- Clinical Approach
- Diagnosis
- Evaluation and Management
- Pearls
- Knowledge Check
- Resources
- Core 1 (Pre-Clerkship)
- Biomedical Science
- Anatomy and Imaging
- The Alimentary Tract and GI Circulation
- POCUS
- Anatomy and Imaging
- Biomedical Science
- Core 2 (Clerkship)
- Pediatric Emergency Medicine Optional Reading - CDEM Approach to Pediatric Abdominal Pain
- Core 3 (Post Clerkship) Electives that may further knowledge - Peds EM
History
- Loss of appetite
- Abdominal pain – can be periumbilical in early stages, but typically located in the right lower quadrant
- Vomiting – usually after the onset of pain
- Fever – usually 24-48 hours after symptom onset
- Diarrhea
- Lethargy/irritability
Physical Exam Findings of Acute Appendicitis
|
Exam Finding |
Description |
|
Significant Pain with Movement |
Severe pain elicited by cough, hopping, or when the examiner bumps the exam table or soles of the patient’s feet |
|
Involuntary Muscle Guarding |
Reflex tightening of the abdominal muscles during palpation |
|
Rebound Tenderness |
Pain increases when steady pressure applied to the RLQ for 10–15 seconds is suddenly released |
|
Percussion Tenderness |
Pain elicited by gentle tapping or percussion over a tender area, suggesting peritonitis |
|
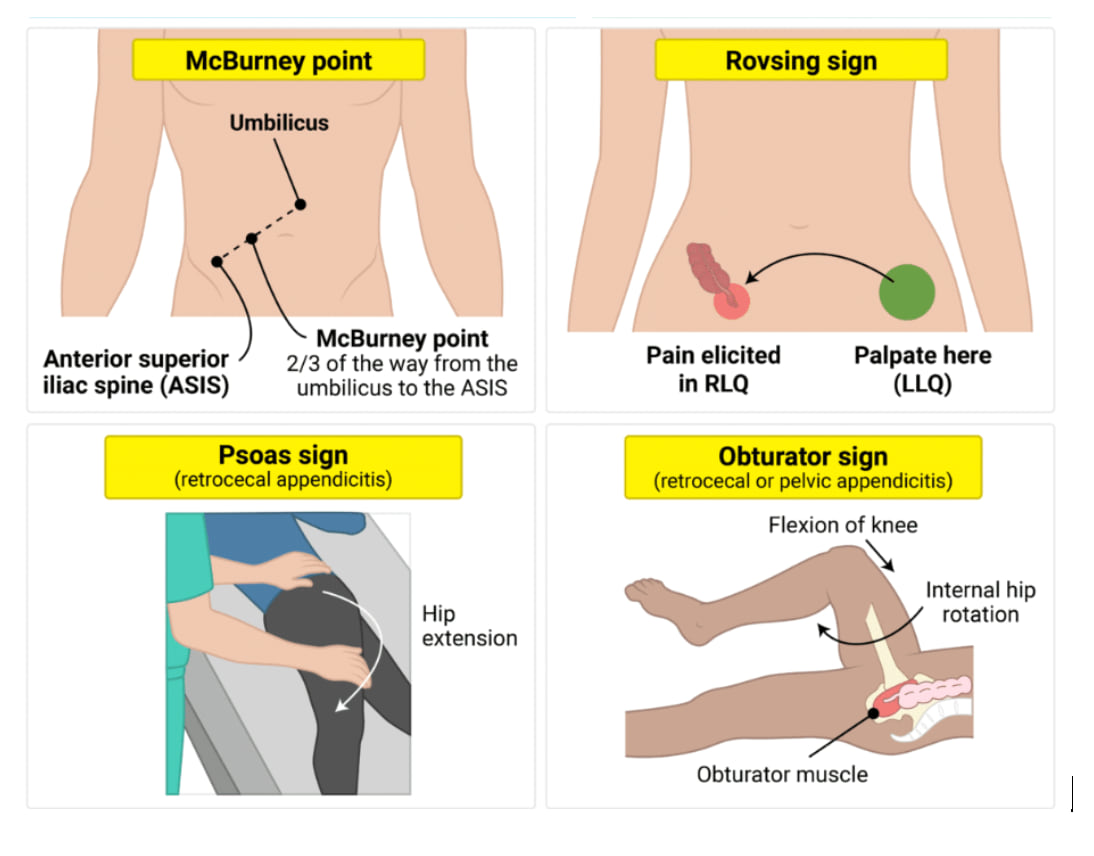
McBurney’s Point Tenderness |
Localized tenderness with some rigidity at a point one-third the distance from the anterior superior iliac spine to the umbilicus; most reliable sign of appendicitis |
|
Rovsing's Sign |
Pain in RLQ when palpating the left lower quadrant, sign of peritonitis |
|
Obturator Sign |
Pain on flexion and internal rotation of the right hip, indicating irritation of the obturator internus muscle due to a pelvic appendix |
|
Iliopsoas Sign |
Pain on extension of the right hip, indicating retrocecal appendicitis |
Source: Rapid Review: Appendicitis - RoshReview.com
The image illustrates four classic appendicitis exam findings. McBurney point tenderness is located two-thirds of the way from the umbilicus to the ASIS; Rovsing sign is pain in the right lower quadrant when palpating the left lower quadrant; the Psoas sign shows pain with hip extension; and the Obturator sign elicits pain with flexion of the knee and internal rotation of the hip. Each diagram shows the relevant anatomy and maneuver to help identify appendiceal irritation.
Risk stratify for appendicitis based on symptoms and labs: Pediatric Risk Calculator or CHOP pathway definitions
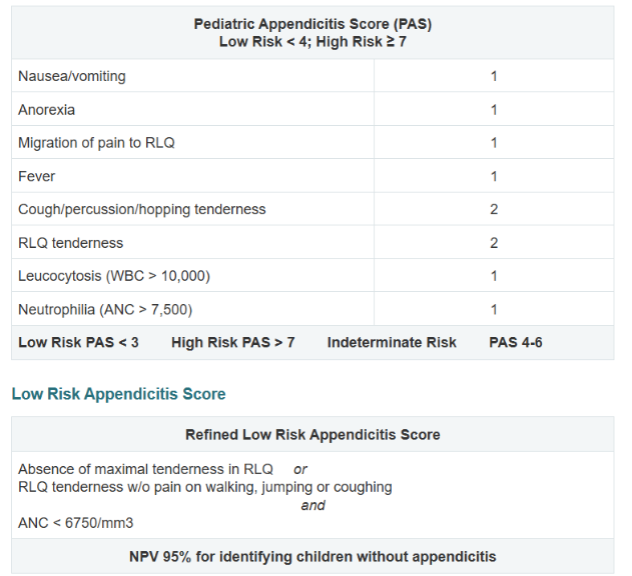
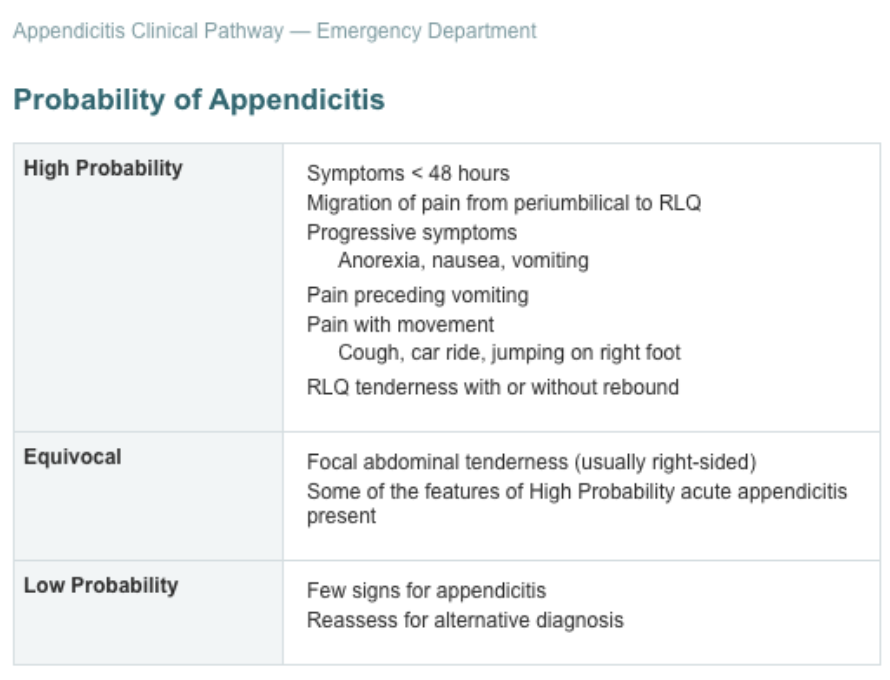
Source: CHOP appendicitis pathway
Evaluation
- Consider laboratory workup for further evaluation in equivocal cases
- CBC, BMP, CRP, UA, pregnancy
- Other workup is dependent on other differential diagnoses
- Imaging for diagnosis in high probability cases
- RLQ Ultrasound – First Line
- MR Appendix
- First line if weight >100kg due to difficulty visualizing appendix on ultrasound with larger body habitus
- Second line if secondary signs of appendicitis on US, but appendix is not seen
Management of appendicitis
- NPO + IVF as clinically indicated
- Surgical consultation for appendectomy
- Antibiotics in cases of perforation and post-operative abscess – typically ceftriaxone and metronidazole
- For post-operative abscess, 7-day course of antibiotics (discharge on oral ciprofloxacin and metronidazole)
- For cases of perforated appendicitis with abscess
- Delay appendectomy
- Consider drainage by interventional radiology + 14 day course of antibiotics
- Interval appendectomy in 4-6 weeks
- Antibiotics in cases of perforation and post-operative abscess – typically ceftriaxone and metronidazole
- Symptoms of appendicitis may be non-specific in younger children and pain may not be located in the right lower quadrant
- Specific exam maneuvers such as McBurney’s point, Rovsing sign, Psoas sign, and Obturator sign may help to assess for appendicitis
- Ultrasound is usually the first line diagnostic test followed by MRI if non-diagnostic
- Most common causes include fecalith, undigested food, or foreign material
- Less common causes include enteric pathogens that can cause lymphoid hyperplasia with obstruction - Adenovirus, measles, EBV
- Most common in age 11-20 years old
- Higher rate of perforation on presentation in younger children likely due to non-specific symptoms in younger children
Click the drop down to reveal the correct answers
Q1: What is the most common age range for appendicitis?
Q2: What is the most reliable physical exam finding for appendicitis?
Q3: A patient has RLQ pain when the left lower quadrant is palpated. What is this sign called and what does it suggest?
Q4: Why is appendicitis often missed in children under 5 years old, and what is a potential consequence?
Q5: A child has RLQ pain worsened by hip extension. What is this sign and what does it suggest?
Q6: When is MRI preferred over ultrasound for diagnosing appendicitis?
Q7: What imaging modality is first-line for suspected appendicitis in pediatric patients?
Q8: In a post-pubertal female with abdominal pain, what conditions must be ruled out before diagnosing appendicitis?
Q9: What antibiotics are typically used for perforated appendicitis?
Answers
Q1: 11–20 years old
Q2: Answer: McBurney’s point tenderness — located one-third the distance from the anterior superior iliac spine to the umbilicus.
Q3: Rovsing’s sign, suggesting peritoneal irritation due to appendicitis.
Q4: Symptoms may be non-specific or atypical, leading to delayed diagnosis and higher perforation rates (up to 100%).
Q5: Iliopsoas sign, suggesting a retrocecal appendix irritating the psoas muscle.
Q6: If the appendix is not visualized or in patients >100 kg with equivocal ultrasound findings. MRI provides better visualization in patients with higher body habitus or unclear US results.
Q7: Right lower quadrant abdominal ultrasound.
Q8: Ectopic pregnancy and ovarian torsion — check urine pregnancy test and consider pelvic ultrasound with Doppler.
Q9: Ceftriaxone and metronidazole.

