Bleeding disorders
A 14-year-old male with no significant past medical history presents to the Emergency Department with a large, swollen knee.
He says that for the past week, he has been on a wilderness trip with his fellow scout troop members. Earlier this morning, he had been gathering wood and slipped on slick forest floor, hitting his left knee. Over the past 8 hours, his knee has become larger in size due to swelling and is hot and very tender to touch. He took some Ibuprofen to help with the pain but reports limited relief. He denies any head trauma, fevers, rashes, or tick bites. He states that he otherwise is feeling okay but is feeling a little dehydrated given that he hasn’t been drinking as much water as he normally does.
He reports that outside of this wilderness trip, he has been eating and drinking as usual. He has not had any joint injuries or fractures before. He reports occasional nosebleeds, but denies excessive bleeding with papercuts and gum bleeding. He is uncircumcised and has never had any sexual activity. He is unaware of any family history of bleeding disorders.
- Joint effusion of the left knee during acute phase of injury | Download Scientific Diagram
- Mucosal Dryness - an overview | ScienceDirect Topics
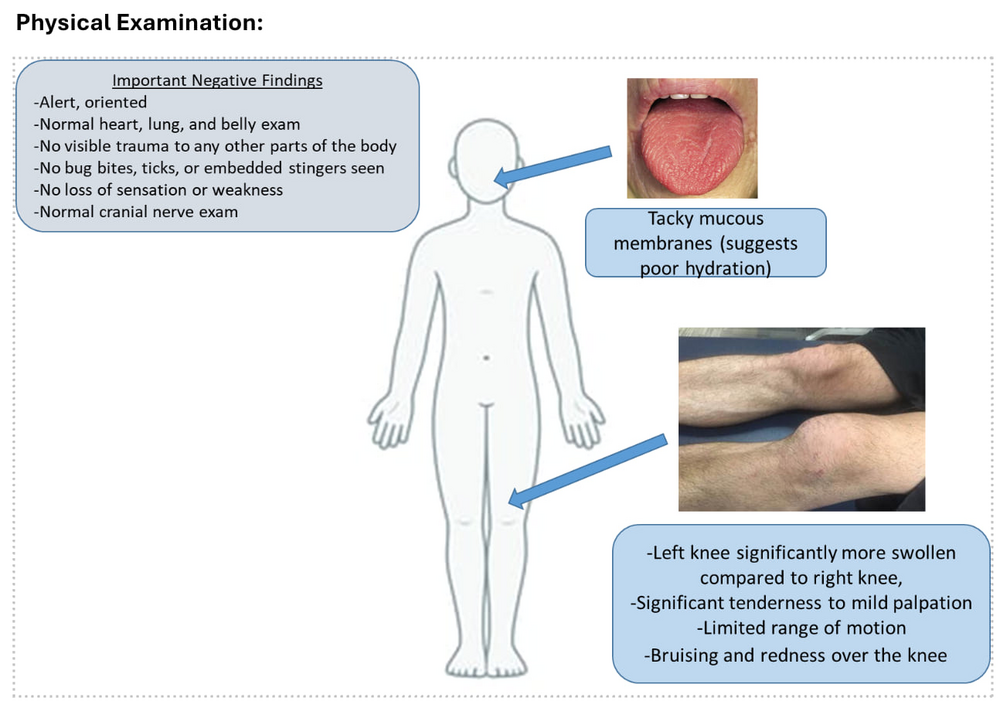
The image shows a child’s exam with notable findings highlighted: tacky mucous membranes suggesting dehydration and a markedly swollen, tender left knee with bruising, redness, and limited range of motion. A text box lists important negative findings, including normal heart, lung, abdominal, and neurologic exams, no visible trauma elsewhere, and no sensory deficits. The overall impression is an isolated joint abnormality in an otherwise stable, alert child.
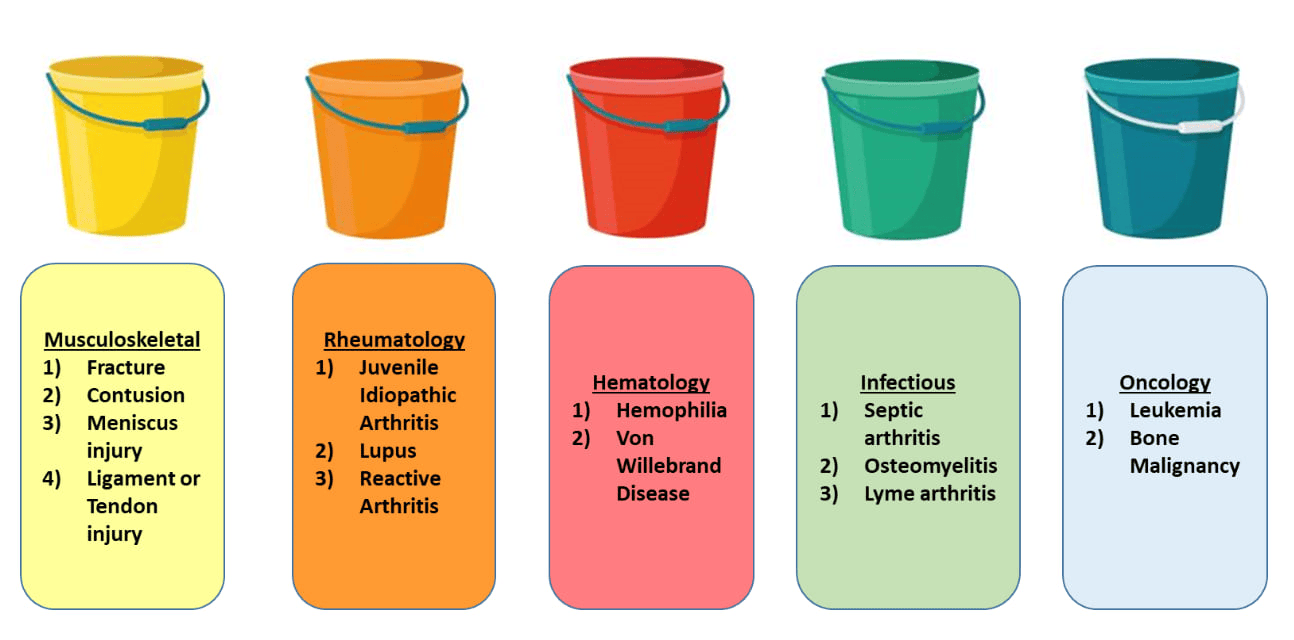
The image uses five different colored buckets to organize the differential diagnosis for a painful or swollen joint. Categories include musculoskeletal injuries such as fractures and ligament tears, rheumatologic conditions like JIA and lupus, hematologic causes such as hemophilia and von Willebrand disease, infectious causes including septic arthritis and osteomyelitis, and oncologic concerns like leukemia or bone tumors. The buckets visually emphasize a structured approach to broad diagnostic possibilities.
Initial Evaluation
- Obtain ultrasound of right knee. Consider MRI of right knee (X-Ray is less sensitive to early changes)
Ultrasound Results
- Ultrasound showed hemarthrosis of the affected knee
Case Progression
- Labs are obtained – complete blood count (CBC), coagulation markers (PT/INR, PTT), von Willebrand factor levels, and blood chemistry panel (BMP).
- Labs show prolonged PTT, Factor VIII activity diminished to 4%, normal von Willebrand factor, and evidence of mild dehydration (increased Cr and BUN) on BMP.
Diagnosis
Hemophilia A! This is a deficiency in clotting factor VIII
How we got there: Given that this patient was found to have Factor VIII of 4%, this is classified as having moderate Hemophilia A. Hemophilia A is classified into mild (5-40% of expected Factor VIII activity), moderate (1-4% of expected Factor VIII activity), and severe (<1% of expected Factor VIII activity). Given that factor VIII is within the intrinsic pathway of the coagulation cascade (which is measured by PTT or prothrombin time), we would expect there to be PTT prolongation, which this patient demonstrated.
Management
- Administer Factor VIII repletion to replace the factor deficiency
- Hematology consult - patients with factor deficiencies should be followed by Hematology, and they will provide prescription for emergency factor repletion at home)
- Physical Therapy consult to ensure the patient does not have deconditioning of knee during acute phase
- Consider DDAVP (stimulates factor VIII release from endothelial cells)
- Consider MRI of right knee for dedicated imaging
- Minimize use of NSAIDs given (reversible) anti-platelet activity
- Consider a broad differential diagnosis when a patient is presenting with a swollen joint
- Hemophilia A is inherited in an X linked recessive pattern
- Obtain thorough personal and family history of bleeding disorders (in males, often diagnosed at time of circumcision)

The chart illustrates the intrinsic and extrinsic pathways of secondary hemostasis and how they converge into the common pathway to form a stable fibrin clot. Each clotting factor is shown activating the next in sequence, with key deficiencies labeled for conditions such as hemophilia A, B, and C, von Willebrand disease, and vitamin K deficiency. A small diagram of a fibrin clot reinforces the end result of the cascade.
Click the drop down to reveal the correct answers
Q1: What is the role of DDAVP in Factor VIII deficiency?
- Inhibits Factor VIII release from endothelial cells
- Increases ability to urinate, thereby decreasing fluid accumulation
- Stimulates Factor VIII release from endothelial cells
- Inhibits platelet activity
Q2: Bob has no family or personal history of hemophilia. Janice does not have hemophilia, but her father had Hemophilia A. If Bob and Janice have a son, what percent chance is there that he will have Hemophilia A?
- 0%
- 25%
- 50%
- 75%
- 100%
Answers:
Q1: C
Q2: C