Celiac Disease
- Where to Find in the PSOM Curriculum
- Clinical Approach
- Evaluation and Management
- Pearls
- Knowledge Check
- Resources
- Core 1 (Pre-Clerkship)
- Integrative Systems
- Gastroenterology: Pediatric Tutorial Cases
- Integrative Systems
- Core 2 (Clerkship)
- Pediatric didactics: Nutrition didactic
- Core 3 (Post Clerkship) Electives that may further knowledge - Peds GI
|
Intestinal Manifestations |
Extra-intestinal Manifestations |
|
Persistent diarrhea |
Neurological/behavioral: headache, irritability, chronic fatigue |
|
Poor weight gain |
Osteopenia/Osteoporosis |
|
Iron/vitamin deficiencies |
Abnormal liver tests (liver disease) |
|
Abdominal pain/distention |
Pubertal delay, slowed height velocity |
|
Constipation |
Dermatitis herpetiformis rash |
|
Vomiting |
Permanent teeth dental enamel hypoplasia |
*NOTE: May also be asymptomatic
- Rarely can present as celiac crisis – acute onset and rapid progression of GI symptoms attributable to celiac disease that often progresses to multi-organ dysfunction
-
- Symptoms can include: severe dehydration, renal dysfunction, neurologic dysfunction, metabolic acidosis, abnormal electrolytes, hypoalbuminemia, weight loss, need for parenteral nutrition
Serologic Evaluation
- Criteria to test: MUST be on gluten-containing diet (ideally 3-6g of gluten for 8-12 weeks). Can consider gluten challenge if diagnosis needs to be made, but the child is already on a gluten-free diet.
|
Celiac Serologies |
||
|
Serology |
Sensitivity/Specificity |
Usage |
|
Tissue transglutaminase antibody (tTG-IgA)* |
90-100%/95-100% |
First-line test |
|
Endomysial antibody (EMA-IgA)* |
93-100%/95-100% |
Second-line test (similar sensitivity/specificity, but subject to interpretation error) |
|
Deaminated gliadin antibody (DGP-IgG) |
88-95%/86-98% |
Check in addition to tTG-IgA for less than 2yo (more sensitive) |
*Check with total IgA given higher prevalence of IgA deficiency with celiac disease. Low IgA can make IgA antibody testing falsely negative. Check tTG-IgG ab if low IgA.
- If antibodies are positive, refer to pediatric gastroenterology for consideration of endoscopy.
- Still refer to GI if high suspicion for celiac disease even if antibodies are negative
- If on a gluten-free diet and unable to do gluten challenge, can consider HLA genetic testing. If HLA-DQ2/DQ8 negative, then celiac disease is unlikely.
Endoscopic Evalution
- Visual findings on endoscopy
-
- Can be visually normal, but findings may include scalloping of the small bowel, prominence of blood vessels, nodularity, flattening of the villi, and ulcers
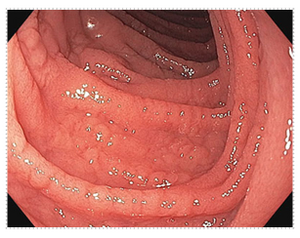
Endoscopic image of small intestinal mucosa with abnormal appearance consistent with celiac disease.
Histology Grading (Marsh Classification)
-
- Celiac is patchy and needs an adequate number of biopsies for diagnosis
- Marsh 3 is definitive for diagnosis of Celiac Disease
- Degree of the villous atrophy does not necessarily correlate with severity of clinical symptoms
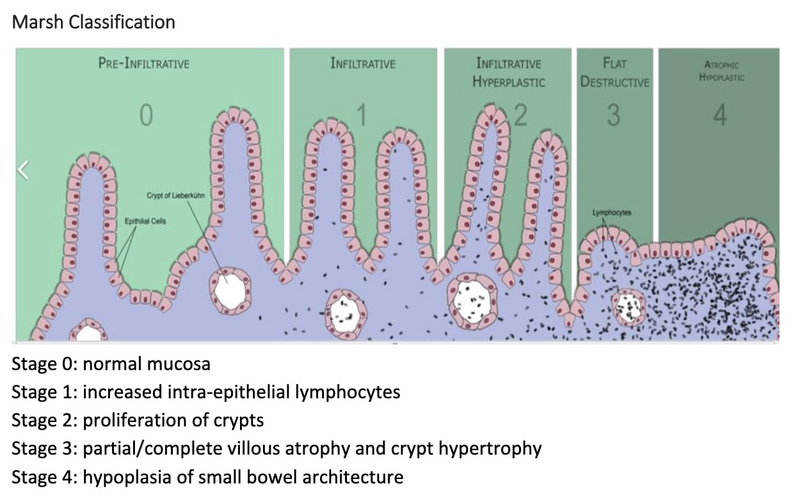
Illustration of the Marsh classification for celiac disease and an endoscopic image showing abnormal small intestinal mucosa.
European Diagnostic Criteria
- In North America, diagnosis of celiac disease requires positive biopsies
- In Europe (ESPGHAN) criteria, diagnosis can be made on serologies alone
-
- tΤG-ΙgA >10 times the upper limit of normal and positive ЕΜA-ΙgΑ from a separate blood draw
Management
- Strict, lifelong gluteո-free ԁiet is the only treatment for celiac disease
- Treatment is should be guided by a dietician
- Gluten is a protein found in wheat, barley, and rye
- If products contain gluten, it is not required to be labelled as gluten containing
-
- Gluten free labelling is voluntary, not required
-
- Families must learn to read labels closely to identify gluten-containing ingredients
-
- Products that contain wheat are required to be labelled as it is one the top 9 food allergens, but this does not encompass all gluten containing foods.
- Non-food items may contain gluten too (makeup, mouthwash, toothpaste, stamps, envelope glue, play dough, vitamins/medicines, etc). Anything that goes into the mouth must be gluten free!
- Families are counselled to avoid cross contamination of gluten/non-gluten condiments and kitchen items
- Diagnosis of celiac disease is made on biopsy from endoscopy
- Asymptomatic screening is indicated in certain high-risk individuals (first-degree relatives, Trisomy 21, Type 1 Diabetes, Williams Syndrome, Turner Syndrome, autoimmune thyroiditis)
- First-degree relative of person with celiac disease
- Other autoimmune disease: autoimmune thyroiditis, Type I DM
- Genetic syndromes: Down syndrome, Turner Syndrome, Williams Syndrome
- IgA deficiency
- In many of these high-risk patients, asymptomatic screening is performed and may need to be repeated over time
- Mainstay of treatment is strict adherence to a gluten-free diet
- Celiac disease is an immune-mediated inflammatory disease in the small intestine in response to gluten
- Celiac disease is not an IgE mediated allergy, but rather an autoimmune disorder where gluten causes activation of an immune cascade resulting in damage to the intestines.
- Occurs in genetically susceptible individuals that have HLA-DQ2 and/or HLA-DQ8 (these play a role in antigen presentation/immune system activation)
- Prevalence is approximately 1:80 to 1:300 children (~1% of the population)
Click the drop down to reveal the correct answers
Q1: How is celiac disease diagnosed?
Q2: A child has positive tTG-IgA, but low total IgA. What should be your next step in serologic testing?
Q3: What HLA genotypes are needed for the development of celiac disease?
Q4: In which populations is asymptomatic screening for Celiac Disease recommended?
Q5: What is the first-line serologic test for celiac disease?
Q6: What lab tests should be sent to screen for celiac disease in children < 2 years old
Q7: What is the only effective treatment for celiac disease?
Q8: Name two extra-intestinal manifestations of celiac disease.
Q9: Is gluten-free labeling mandatory in the U.S.?
Answers
Q1: EGD evaluation with biopsy findings of villous atrophy and crypt hypertrophy (Marsh 3 classification)
Q2: Order tTG-IgG, since IgA deficiency may cause false-negative tTG-IgA results
Q3: HLA-DQ2 and/or HLA-DQ8 – involved in antigen presenting. If negative, risk of celiac disease is close to zero.
Q4: First-degree relatives, and children with Type 1 Diabetes, Down syndrome, Turner syndrome, Williams syndrome, autoimmune thyroiditis
Q5: tTG-IgA. High sensitivity/specificity; always check total IgA due to IgA deficiency risk.
Q6: tTG-IgA, total IgA, AND DGP-IgG (increased sensitivity in children < 2 years old)
Q7: What is the only effective treatment for celiac disease?
Q8: Dermatitis herpetiformis, dental enamel hypoplasia, liver disease, neurologic/behavioral changes (headaches, irritability, chronic fatigue)
Q9: No, it’s voluntary, so families must be counseled on how to read packaging.

