Constipation
- Where to Find in the PSOM Curriculum
- Clinical Approach
- Key Concepts
- Treatment
- Pearls
- Knowledge Check
- Resources
- Core 1 (Pre-Clerkship)
- Core 2 (Clerkship)
- Core 3 (Post Clerkship) Electives that may further knowledge - Peds GI, Peds SubI
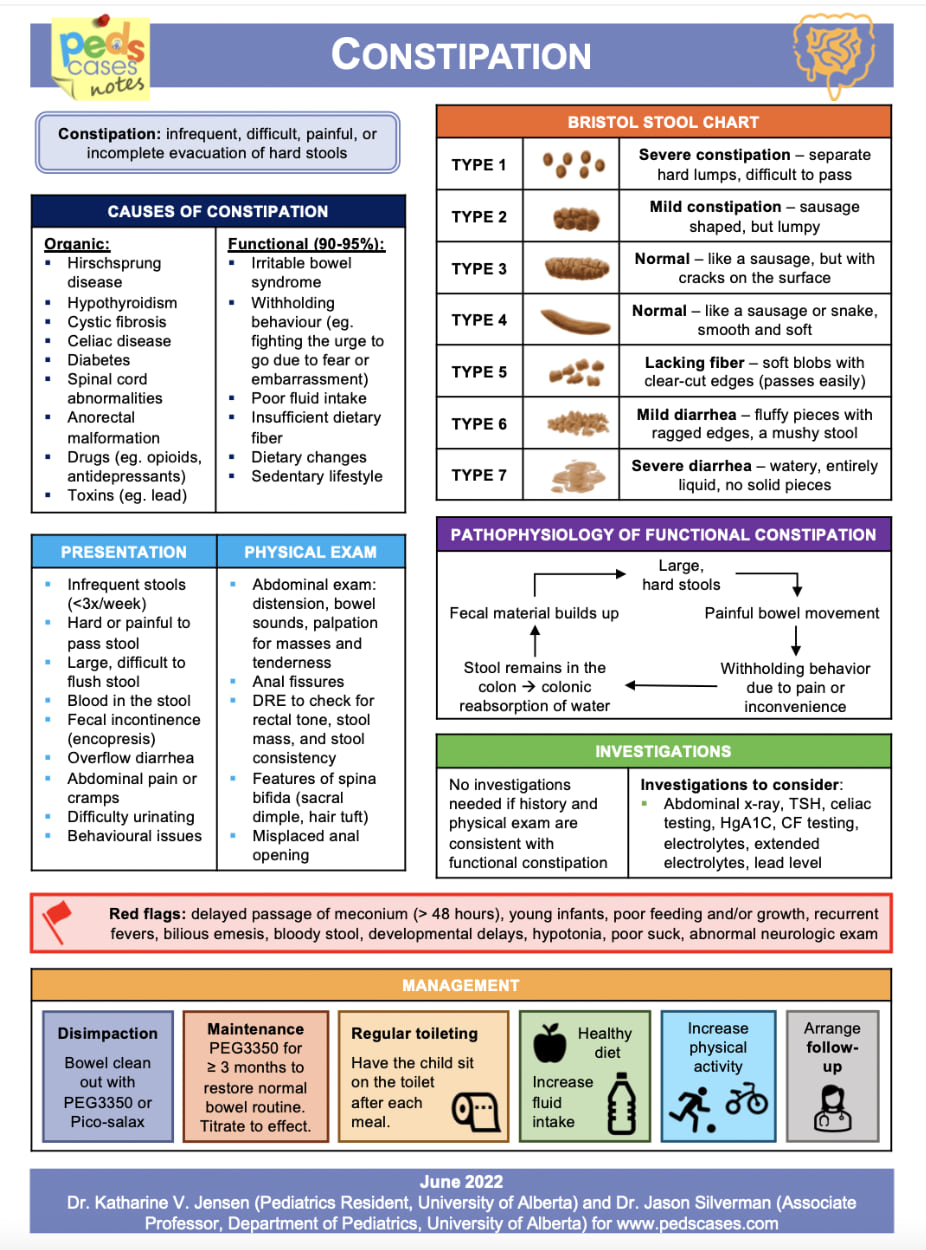
- The goal of the initial assessment for constipation is to elicit history/physical exam findings consistent with functional constipation and red flag signs that are concerning for organic etiologies for constipation that may require further workup.
- Patients with functional constipation may be able to cite a specific triggering event or will describe clear withholding behaviors (squeezing/crossing legs [some parents misinterpret this as straining or trying to go to the bathroom], hiding in a corner, rocking back and forth)
- Triggering Events:
-
- Infancy (6mo-1yo) - Diet change: Starting solids, introduction of cow’s milk
-
- Toddler age (2-3yo) - Toilet training
-
- Pre-school/School age (3-5yo) – Starting school, retentive pattern due to inconvenient/uncomfortable situations
-
- Big life changes/stressors - birth of a new sibling, moving, family changes
|
ALARM SIGNS |
|
|
History/Exam Findings |
Possible Implications |
|
Delayed passage of meconium (after 48h of life), onset in early infancy |
Congenital causes: Hirschsprung disease (HD), cystic fibrosis (CF), anatomic problems, pseudo-obstruction, neurologic causes |
|
Weight loss, poor weight gain, delayed growth |
Systemic causes: HD, hypothyroidism (especially delayed growth), celiac disease, CF |
|
Abdominal distention, bilious/persistent vomiting. For distal obstruction, may have tight rectal tone or abnormally placed anus. May have small diameter, “ribbon” stools. |
Obstructive causes Anatomic: Anal stenosis, intestinal stricture, ectopic/anterior anus Motility: chronic intestinal pseudo-obstruction, HD Other: meconium ileus (CF) |
|
Regression of milestones, urinary incontinence. On exam, pelvic mass (sacral teratoma), lower spine anomalies, lumbosacral dimple, hair tuft, deviation of gluteal cleft, absent anal wink, absent cremasteric reflex, abnormal lower extremity DTR, decreased LE strength |
Neurologic causes: tethered cord, spinal cord tumor, meningomyelocele, spinal cord anomaly Other general causes with neurologic manifestations: lead poisoning |
|
Acute episode of fever, vomiting, lethargy, abdominal distention, or diarrhea |
HD-associated enterocolitis |
|
Rectal bleeding |
Anal fissure, food protein-induced proctitis (milk protein intolerance), IBD, infectious colitis, HD-associated enterocolitis |
|
Urinary incontinence or bladder disease |
Congenital or acquired neurologic deficit (e.g., sacral teratoma), CAKUT (which may be associated with HD), abdominal mass effect, or pseudo-obstruction |
|
Explosive expulsion of stool after digital examination of the rectum |
HD |
|
Extreme fear during the anal inspection |
Sexual abuse |
|
Not responsive to standard constipation therapy |
Underlying organic disease, non-adherence to regimen |
- Pathophysiology – Passage of a painful stool is a trigger for withholding. Once a child knows that it is painful to stool, they will do anything they can to avoid stooling and the stool accumulates in the rectum. This makes the stools harder/larger and stretches the rectum, which alters defecation dynamics and can make it hard to sense when the rectum is full. This leads to an escalating cycle of constipation/hard stools re-enforcing behaviors that make constipation worse.
- ROME Criteria Definition for > 4 years old: At least 2 weeks of 2 of the following:
-
- Two or fewer stools in the toilet per week
-
- At least one episode of fecal incontinence per week
-
- History of retentive posturing or excessive volitional stool retention
-
- History of painful or hard bowel movements
-
- Presence of large fecal mass in the rectum
-
- History of large diameter stools which may obstruct the toilet
- Encopresis can sometimes be the presenting symptom
- Severe constipation can occasionally progress to urinary incontinence due to mass effect of stool burden pushing on the bladder and weakening of the pelvic floor muscles
- In infants < 6 months old, constipation can be confused with infant dyschezia, which is defined as at least 10 minutes of straining and crying followed by successful or unsuccessful passage of soft stool in an otherwise healthy infant. This is caused by discoordination of stooling mechanics when trying to stool. This resolves spontaneously over weeks to months.
- Keep track of stool consistency, frequency, size, and associated symptoms to track progress. Bristol stool chart can be helpful to help children describe stools.
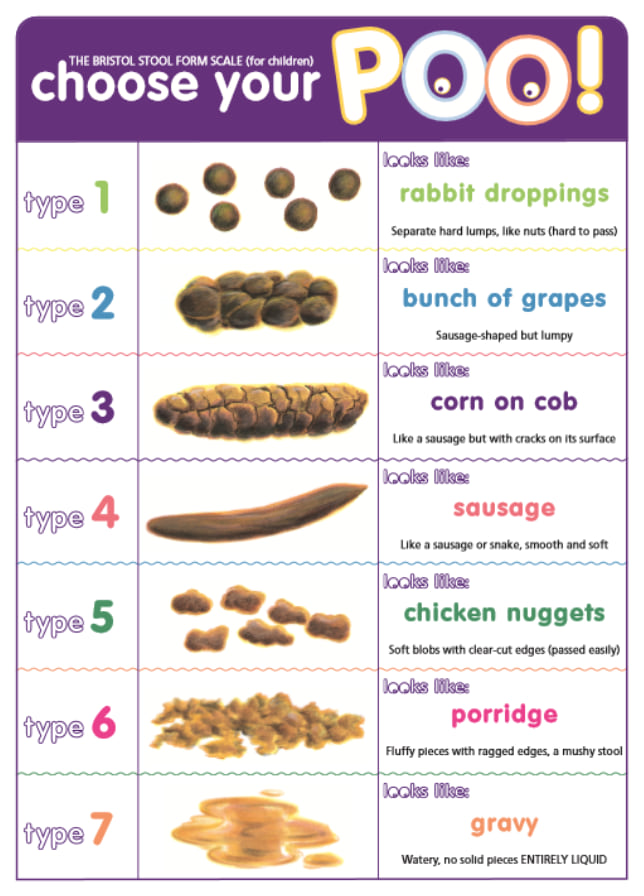
This poster illustrates the pediatric Bristol Stool Scale, pairing each of the seven stool types with visual examples and playful comparisons like “rabbit droppings,” “corn on the cob,” “sausage,” “porridge,” and “gravy.” Types range from hard, pellet-like stools (constipation) to entirely liquid stools (diarrhea). The goal is to help children describe their stool form in an accessible, easy-to-understand way.
- Treatment can consist of large “bowel clean-out” and/or maintenance therapy. See CHOP constipation pathway.
- Large “bowel clean out” typically involves large amount of osmotic laxative, typically polyethylene glycol +/- stimulant laxative/rectal therapies to clear the bowel of stool. Most useful with fecal impaction or severe chronic constipation
- Maintenance treatment of chronic functional constipation should be done consistently for at least 2 months in order to help the child “re-learn” that stooling is not painful and to allow the time for the rectum to shrink back down and regain function
- Osmotic laxatives are generally first line agents for constipation
- Stimulant laxatives are generally used as adjuncts to osmotic laxatives
- Rectal therapy is most useful for those with distal fecal impaction. Use with caution as traumatic administration can worsen/reinforce withholding behaviors
- Treatment should always incorporate behavioral modifications (for toilet trained)
- Consider treatment of comorbid psychological conditions: ADHD, Autism
- If triggered by toilet training, hold off on toilet training until after constipation is under control.
|
COMMON TREATMENTS FOR FUNCTIONAL CONSTIPATION |
||||
|
Osmotic Laxative – Mechanism of Action (MOA): draws water through osmotic forces into the lumen to soften stool and help it move through the colon |
||||
|
Agent |
Administration |
Pros |
Cons |
Notes |
|
Lactulose (1st line) |
Liquid |
Tastes good, safe to use in < 6mo |
Gassiness |
|
|
Polyethylene glycol (1st line) |
Dissolvable powder mixed in clear liquid |
Works well, not systemically absorbed, well tolerated |
Large volume (6-8oz), Min age > 6 mo |
Historic research report linking to Autism. Despite being later redacted, this is still believed by some. There has been NO evidence that this is true. |
|
Magnesium Products (2nd line) |
Dissolvable powder, chews/gummies, pills |
Multiple formulations |
Careful with renal impairment – can cause accumulation/toxicity |
|
|
Docusate |
Pills, chews, liquid |
Multiple forms |
Not typically as effective as other agents |
|
|
Stimulant Laxatives – MOA: works to stimulate contraction of the bowel to move stool through the colon |
||||
|
Agent |
Administration |
Pros |
Cons |
Notes |
|
Senna |
Liquid, ex-lax chocolate squares, pills |
Effective, multiple formulations |
Can cause blistering diaper rash (use with caution if not toilet trained). May cause abdominal cramping. |
Some patients will use senna tea, but dose/effect can vary, so pharmaceutical preparations are preferred |
|
Bisacodyl |
Pill |
Stronger contractions |
≥ 3 yo. Must be taken whole (enteric coated), can cause abdominal cramping |
|
|
Rectal Therapies – MOA: distends the rectum causing it to relax to let stool out, some have active stimulant ingredients |
||||
|
Agent |
Administration |
Pros |
Cons |
Notes |
|
Glycerin suppository |
Rectal |
Okay for <1yo, smaller volume |
Can develop dependence, not as effective as enemas |
|
|
Bisacodyl suppository |
Rectal |
Stimulant effect, smaller volume |
≥ 2yo. Not as effective as enemas, cramping |
|
|
Sodium Phosphate Enema |
Rectal |
Stimulant effect |
≥ 2yo. Risk of hyperPhos in <2 years old and with repeated use |
Pediatric enema is ½ volume of adult sized enema. Often labelled as “saline enema” in stores |
|
Sodium Chloride Enema |
Rectal |
Lower risk of side effects |
>1yo. Only available inpatient. May not be as effective as sodium phosphate enema. |
Sodium chloride enemas are not commercially available for purchase over the counter or outpatient |
|
Mineral Oil Enema |
Rectal |
Good for lubrication of hard stool ball. |
≥ 2yo. Can stain clothes. No stimulant effect |
Usually done prior to sodium phosphate enema rather than as monotherapy. Only sold in adult size/volume over the counter |
|
Dietary Changes – MOA: similar to osmotic laxatives, work to draw fluid into the lumen |
||||
|
Agent |
Administration |
Pros |
Cons |
Notes |
|
Prunes/Pears/ Apples |
Juice/purees |
Well tolerated taste, widely available |
High sugar |
Can use diluted juice to minimize sugar. Can give smaller volumes in < 6 mo. Can use purees once ≥ 6mo |
|
Fiber |
Powder, pills, gummies, food |
Natural treatment |
Too much can cause constipation and gas |
Grams of fiber = Age + 5 |
|
Water |
N/A |
N/A |
Difficult compliance |
Calculated daily mIVF volume is a good rough estimate |
|
Behavior Modifications – MOA: works to improve defecation dynamic and prevent withholding |
||||
|
Behavior |
Strategies |
|||
|
Toilet sitting |
Time: Age in minutes up to 10 minutes Tips for success: Do 10-15 minutes after meals (gastrocolic reflex), sticker chart/positive reinforcement, sitting up straight, feet flat on a stool, blow on pinwheel/bubbles to engage abdominal muscles, no distractions/ipad |
|||
|
Exercise |
Any intensity is okay. Do something the child enjoys |
|||
|
School Accommodation |
Free access to bathroom, private bathroom, toilet sits, free access to water, medications at school, assistance with toileting. Can ask for a 504 Plan. |
|||
- Ask about “red flags” for organic causes of constipation
- Osmotic laxatives are the first line treatment for constipation
- Always pair behavioral interventions/teaching with medical therapy
Click the drop down to reveal the correct answers
Q1. What is the first-line pharmacologic treatment for functional constipation in children?
Q2. A child has explosive expulsion of stool after digital rectal exam. What diagnosis should be considered?
Q3. A toilet-trained 5-year-old has chronic constipation and new-onset urinary incontinence. Exam shows a sacral dimple and decreased lower extremity reflexes. What is the next step?
Q4. A 5-month-old strains and cries for 10 minutes before passing a soft stool. What is the most likely diagnosis?
Q5. List 2 triggers for the onset of functional constipation.
Q6. A 7-year-old with constipation has recurrent UTIs. What mechanism explains this?
Q7. What constipation medication should be used with caution in non-toilet trained children?
Q8. How much fiber should you recommend for a child with constipation?
Q9. What rectal therapies can be used in children < 2 years old?
Q10. What are the ROME criteria for functional constipation?
Answers
Q1. Osmotic laxatives such as polyethylene glycol (PEG) or lactulose. These agents soften stool by drawing water into the colon. PEG is preferred in older infants/children; lactulose may be used in infants <6 months.
Q2. Hirschsprung Disease (HD).
Q3. Order spinal imaging (MRI). Neurologic findings and lumbosacral cutaneous markers raise concern for tethered cord or other spinal anomaly.
Q4. Infant dyschezia. In infants <6 months, this benign condition is due to discoordination of abdominal and pelvic muscles. Stools are soft, and the infant is otherwise healthy.
Q5.
- Infancy (6–12 months): Starting solids, introduction of cow’s milk
-
Toddler age (2–3 years): Toilet training
-
Preschool/School age (3–5 years): Starting school, withholding behavior
-
Big life changes/stressors: New sibling, moving, family changes
Q6. A large stool burden can impair bladder emptying, leading to urinary stasis and increased risk of UTIs.
Q7. Senna, as it can cause a blistering diaper rash in non-toilet trained children.
Q8. Recommend fiber intake as: age (in years) + 5 grams per day.
Q9. Glycerin suppositories. Enemas are generally not recommended for children <2 years. Avoid Fleet enemas due to risk of hyperphosphatemia.
Q10. ROME IV criteria for children >4 years old: ≥2 of the following for ≥2 weeks:
-
≤2 defecations/week
-
≥1 episode of fecal incontinence/week
-
History of retentive posturing or excessive stool retention
-
History of painful or hard bowel movements
-
Large fecal mass in rectum
-
Large-diameter stools that may obstruct the toilet
Good resources for patients (and you!)
- The Poo in You - Good video for explaining chronic constipation to families/kids

