Disorder of Gut-Brain Interaction
- Where to Find in the PSOM Curriculum
- Clinical Approach
- Differential Diagnosis
- Treatment
- Pearls
- Knowledge Check
- Resources
- Core 1 (Pre-Clerkship)
- Integrative Systems:
- Gastroenterology - Irritable Bowel Syndrome
- Integrative Systems:
- Core 2 (Clerkship)
- Core 3 (Post Clerkship) Electives that may further knowledge - Peds GI, Peds SubI
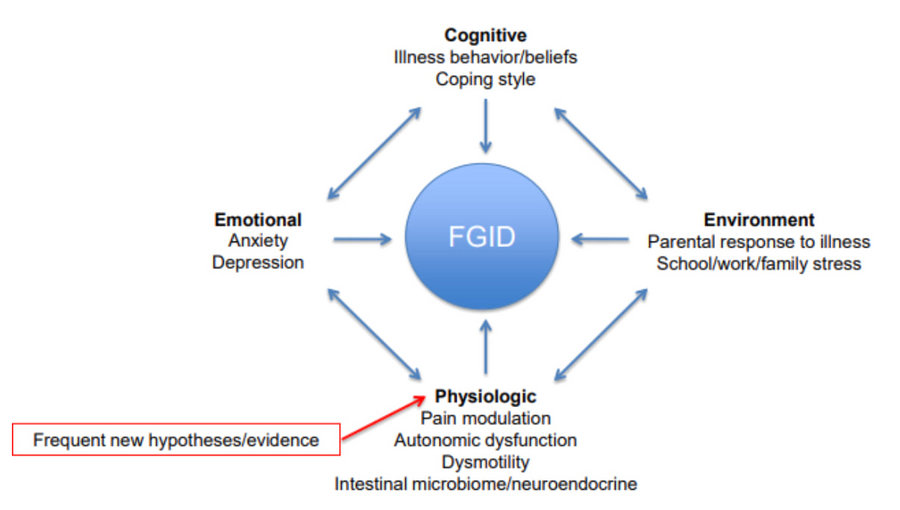
- Chronic abdominal pain without any organic etiology that is thought to be due to a combination of cognitive, emotional, environmental and physiologic factors.
- One of the most common causes of abdominal pain in children (8% of children)
- Highest prevalence in 4-6 years old and in early adolescents
- It is a symptom-based diagnosis. If there are no “red-flags,” very few/no diagnostic tests are needed for diagnosis
 '
'
Source: NASPGHAN Functional Abdominal Pain Lecture
The diagram places FGID at the center and illustrates how multiple domains—cognitive beliefs and coping style, emotional states like anxiety or depression, environmental stressors, and physiologic mechanisms such as pain modulation, dysmotility, or microbiome factors—interact to shape symptoms. Arrows point bidirectionally, emphasizing that each factor can influence and be influenced by the disorder. A note highlights that new physiologic hypotheses and evidence are continually emerging in this area.
ROME IV Criteria (ROME Calculator)
- Symptom based definitions for specific subtypes of DGBI
- Diagnostic criteria can help provide a more tangible diagnosis for both patients/providers
- Certain diagnoses can respond better to different medical therapies
|
ROME IV Criteria for Common Causes of DGBI Abdominal Pain |
|
|
Condition |
Symptoms & Criteria Note: For all diagnoses, symptoms cannot be explained by another medical condition after appropriate evaluation |
|
Functional dyspepsia |
One or more of the following for the at least 4 days/month for at least 2 months:
|
|
Irritable bowel syndrome |
Recurrent abdominal pain on average 1 day/week in the last 3 months with 2 or more of the following:
|
|
Abdominal migraine |
All of the following symptoms occurring at least twice 6 months prior to pain:
|
|
Functional Abdominal Pain – Not Otherwise Specified |
All of the following symptoms at least 4 times per month for at least 2 months:
|
Red Flags For Alternative Diagnoses
|
Red Flag Findings |
Potential Significance |
|
Involuntary weight loss/deceleration in linear growth/delayed puberty |
Malabsorption (IBD, celiac disease, pancreatic insufficiency), malignancy |
|
Significant vomiting (bilious, protracted, projectile, or hematemesis) |
Acid-peptic disease, obstruction, cyclic vomiting syndrome, eosinophilic gastroenteritis, metabolic disorders, increased intracranial pressure, diabetic ketoacidosis, adrenal crisis, cannabis hyperemesis, food protein-induced enteropathy |
|
Chronic severe diarrhea (>3 loose or watery stools per day for more than 2 weeks) or nocturnal diarrhea or bloody stools |
Infection, IBD, celiac disease, food protein-induced enteropathy |
|
Unexplained fevers |
Infectious process; familial Mediterranean fever/fever syndromes, autoimmune disorders, IBD |
|
Arthritis, oral ulcers |
IBD, autoimmune disorders |
|
Urinary symptoms (change in bladder function, dysuria, hematuria, flank pain) |
Recurrent urinary tract infection; nephrolithiasis, mass effect |
|
Back pain |
Referred pain (e.g., chronic pancreatitis), kidney problems |
|
Family history of IBD, celiac disease |
IBD, celiac disease |
|
Melena (black, tarry stools) or hematemesis |
Peptic ulcer, H. pylori, gastritis |
|
Skin changes (rash, eczema, hives) |
IBD, celiac disease, food allergy, autoimmune disorders |
|
Consistent localized pain |
Consider disease of the organ in the location (ie. RUQ disease – gallbladder, lower quadrants – ovarian/GU, etc) |
|
Perianal abnormalities (eg, skin tags, fissures, fistulae) |
Inflammatory bowel disease |
|
Hepatomegaly |
Chronic hepatitis, hepatobiliary disease, storage disease (eg, Gaucher disease) |
|
Splenomegaly |
Hemolytic disease, splenic infarct, splenic abscess, storage disease, chronic hepatitis/portal hypertension |
|
Abdominal mass |
Malignancy |
|
Laboratory abnormalities (ie. Unexplained anemia, leukocytosis, elevated inflammatory makers, markers or organ dysfunction) |
Diagnosis depends on abnormal lab |
Source: AAP and UpToDate
Multimodal biopsychosocial approach is critical! Family buy-in is even more critical!
- Psychotherapy w/ GI Psychologist if available
-
- This can include CBT, breathing techniques, coping skills to deal with pain and contributing mental health disorders
-
- RCTs have shown that children who participate in CBT improved quicker, were more likely to be pain free by 3-months, had higher levels of function, higher levels of satisfaction, and had lower levels of relapse at follow-up
- Medications – limited evidence, and none work very well, often done with GI provider
-
- Anti-spasmodics – hyoscyamine, dicyclomine
-
- Acid blocking medications – PPI/H2 blocker (if dyspepsia symptoms)
-
- Peppermint oil capsules – IBGard, FDGard
-
- Probiotics – lactobacillus
-
- Fiber supplements
- Advanced medications for IBS: linaclotide, prucalopride, eluxadoline
- Neuromodulators
-
- Amitriptyline (lower dose than for depression)
-
- SSRI/SNRIs – used in coordination with psych
-
- Some providers use mirtazapine, buspirone, and other anti-depressants or psych medications
- Headache medications (usually prescribed by a neurologist)
-
- Specifically for abdominal migraines
- Physical Therapy (specifically pelvic physical therapy/biofeedback)
- Dietary
-
- Encourage hydration, regular mealtimes
-
- Avoid any specific food triggers identified
-
- Often avoid significant dietary restriction to prevent restrictive eating
- Can consider FOD-MAP diet in IBS
- Integrative health
-
- Massage
-
- Yoga
-
- Acupuncture
Guide to Talking with Families
Talking to families about DGBI can be difficult! It is hard to not have a positive test to point to for a diagnosis. Families often hear the diagnosis of disorders of “brain-gut interaction” as “I’m making it up” or “It’s all in my head.” Here are some general strategies, analogies, and scripts to help you discuss this diagnosis with families. Ultimately, choose the way that makes the most sense to you!
General Principles:
- Validate that their pain is real/life impairing, but not dangerous
- Mention DGBI early as you would for any other diagnosis in your differential
- Discuss that even though the child is experiencing pain, that the pattern of symptoms is not something that is consistent with a dangerous problem with the organs
- Reassure families that we will always do more testing if indicated based on symptoms
- If impaired function and/or clear anxiety/depression component, discuss psychology early even if still undergoing testing if high suspicion for DGBI
- Set realistic expectations – focus on goal of return of function or decreasing severity of pain to tolerable level rather than complete elimination of pain
- Coach parents not to constantly ask about pain/elicit pain scores
- You do not have to offer all information at the first visit!
Headache
“DGBI is similar to a headache. When you or I get a headache, it is very painful and prevents us from doing our day to day activities. We can have headaches that cause debilitating pain, even when there is nothing wrong with our brain. The same can happen to the gut! Treating headaches and belly pain can be similar. The goal is to help us to manage the symptoms to allow us to go back to our day to day lives!"
Hardware/Software
“I like to think about DGBI as if the body is a computer. A computer can have issues with the physical parts of the computer (the hardware) or the functional parts of the computer (the software). In DGBI, there is nothing wrong with the hardware of the computer (the body/organs), but the software (the nerves of the gut) is malfunctioning, which affects how the computer overall is able to function. The way to treat this is by focusing on strategies that fix the malfunctioning nerves in the gut”
Fire Alarm
“Think about the body as a house and the nervous system as the fire alarm. The nerves are supposed to send pain signals to the brain to warn you when your body interacts with something harmful. Think about how you experience pain when you touch something sharp or hot. Similarly, when a house is on fire, a fire alarm goes off to warn people of danger. But, once the fire is put out, the alarm may still continue to ring even though the fire is gone. The same can happen to our body. Sometimes, our body responds to a trigger that causes pain such as an illness, but the pain continues long after the illness/trigger is gone and the body is safe. It is our job to figure out how to turn off the alarm system and calm down the nerves in the gut”
Temperature
“Have you ever noticed that people have different pain tolerance when it comes to heat? Sometimes when I wash my hands, someone else will feel the water I am using and say “Ouch that is too hot!” That is because everyone’s nerves are different and something that is painful for someone might not be painful for others. The same can happen in your gut! The gut is ALWAYS working. After you eat a meal, it digests and moves the food through hundreds of feet of intestines. Most people don’t notice this, but some people develop sensitive nerves in the gut that interpret the normal activity of the gut as painful. However, there are ways that we can work to quiet the nerves in your gut and help you feel better!”
Treatment
“Besides the brain, the gut has the most nerves in the body! The nerves in the brain and the gut talk to each other – think of how sometimes your stomach hurts when you are nervous about a game or a performance. Much of what we do to help the nerves in the stomach is focused on helping the brain! One of the best treatments that has the most evidence for the treatment of DGBI is cognitive behavioral therapy/psychology. We don’t use psychology because we think the pain is “all in your head” or “made up” because clearly your pain is real and affecting your life and function. However, psychology is a powerful tool to enlist the brain’s help in calming down the nerves in our gut. There are also some medications we can use to help, but each of them works differently for everyone, so there may be a bit of trial and error. In addition to medicines, doing things that are healthy for the body, such as getting enough sleep, drinking enough water, eating regular meals, and exercising can also be helpful. In some cases, it is even helpful to get special pelvic floor therapists to help strengthen and control the muscles around the belly, which can help with pain. Ultimately, the goal is not to make the pain go away entirely, but to get the pain to a level where you can be functional. For your child, I would recommend...”
- Always ask about “red-flag” symptoms and work up appropriately
- Discuss the diagnosis of DGBI early
- Multi-disciplinary approach to treatment of DGBI is essential
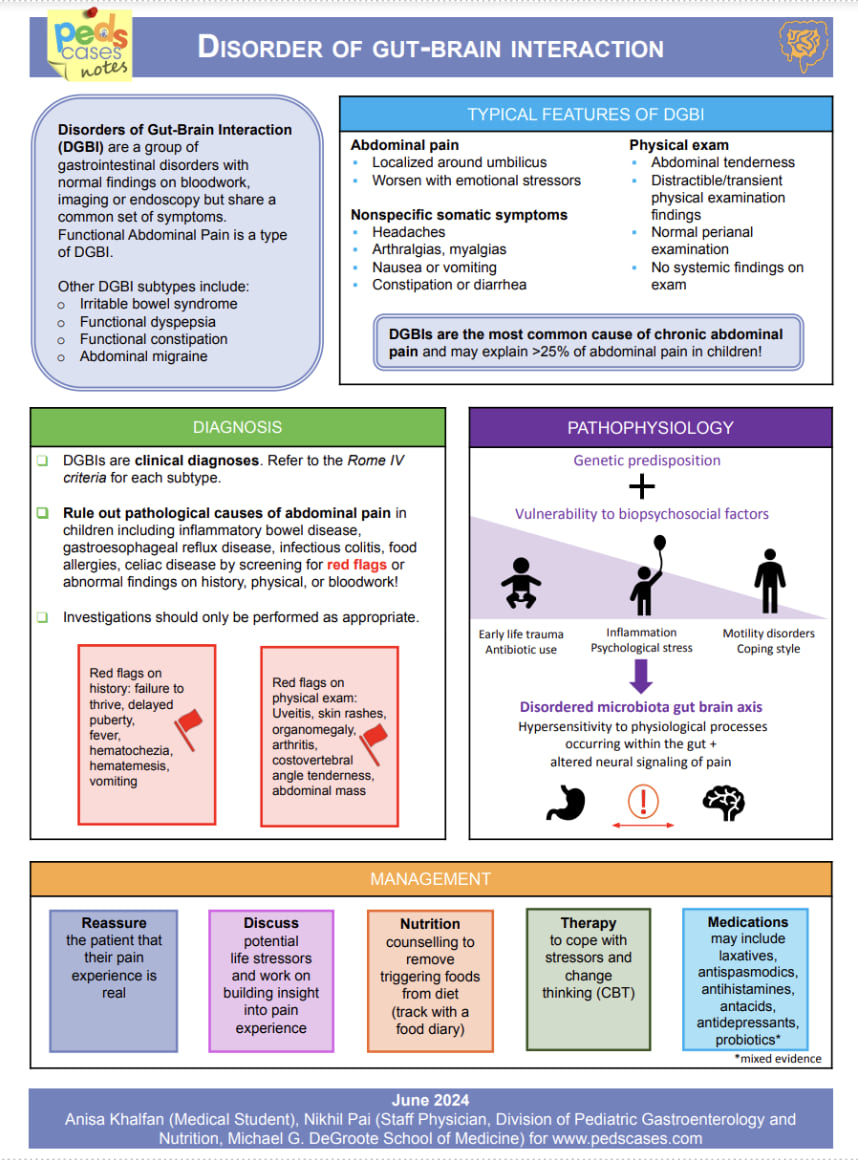
The chart explains that disorders of gut–brain interaction (DGBIs) are functional GI disorders with normal testing but significant symptoms, often presenting with periumbilical abdominal pain, somatic symptoms, and normal physical exam. It outlines diagnostic criteria, emphasizes the importance of ruling out red flags, and describes a biopsychosocial pathophysiology involving genetic predisposition, stress, inflammation, motility issues, and microbiome changes. Management focuses on validation, identifying stressors, nutritional strategies, cognitive-behavioral approaches, and selective medication use.
Click the drop down to reveal the correct answers
Q1. What testing is needed to diagnose DGBI?
Q2. List two red flag symptoms that would prompt further evaluation for organic causes of abdominal pain.
Q3. What is the treatment for DGBI?
Answers
Q1. No lab tests are needed to diagnose DGBI as long as there are no red-flag symptoms.
Q2. Red flag symptoms include:
- Involuntary weight loss or delayed growth
-
Severe vomiting (e.g., bilious or projectile)
-
Chronic diarrhea (more than 3 loose stools per day)
-
Blood in the stool (melena or hematemesis)
-
Urinary symptoms (dysuria, hematuria)
-
Back pain (referred pain or signs of kidney issues)
Q3. Treatment for DGBI involves a multimodal approach, including:
- Cognitive Behavioral Therapy (CBT): To address emotional/psychological components of pain
-
Physical Therapy: Including biofeedback and pelvic floor therapy
-
Integrative health techniques: Such as yoga, massage, and acupuncture
-
Dietary modifications: Including a FODMAP diet to identify and avoid triggers
-
Medication adjuncts: Such as antispasmodics, peppermint oil, fiber, and neuromodulators

