Fever and Limp
- Where to Fnd in the PSOM Curriculum
- Clinical Approach
- Differential Diagnosis
- Evaluation and Management
- Pearls
- Knowledge Check
- Resources
- Core 1 (Pre-clerkship)
- Microbiology and Infectious Disease 1, Week 2: Antibiotics
- Microbiology and Infectious Disease 1, Week 4: Infectious Arthritis
- Core 2 (Clerkship)
- Pediatrics Clerkship didactics on Acutely ill
- Core 3 (Post Clerskhip) Electives that may further your knowledge
- Peds ID, Peds Orthopedics
Clinical Vignette: A 3-year-old presents with 3 days of fever and limping (favoring left leg), now with refusal to bear weight on the left leg. His mother denies any falls or recent known trauma.
History:
- Discuss any known trauma or possibility of unidentified trauma (was child alone with another caregiver such as at daycare?)
- Recent symptoms suggestive of viral illness: cough, rhinorrhea, vomiting, diarrhea
- B-symptoms: fever, unexplained weight loss, night sweats
- Exposures: recent travel, exposure to animals, tick bites/exposure to outdoors in Lyme endemic areas
- Dietary history: does the child eat foods containing adequate vitamin C and vitamin D (concern for scurvy, rickets)?
- Developmental history – when did the child start walking, have they had prior difficulty with gait?
Physical Exam:
- Assess gait as able
- Assess back for tenderness or deformities
- Assess extremities: look for point tenderness over bones, joint swelling, range of motion, be sure to assess all joints of the lower extremity (hip, knee, ankle)
- Assess for lymphadenopathy
- Assess for any rashes
- Assess abdomen: palpate for mass, tenderness, hepatosplenomegaly
- Assess GU: testicular torsion (referred pain → limp)
- Assess neurological exam
The differential for limping in a pediatric patient is quite broad. Below are multiple ways to organize the differential. In the setting of limp + fever, consider the underlined diagnoses
STOP LIMPING mnemonic:
- Septic arthritis (hip or knee)
- Toddler’s fracture
- Osteomyelitis
- Perthes disease (Legg-Calve-Perthe disease)
- Limb length discrepancy
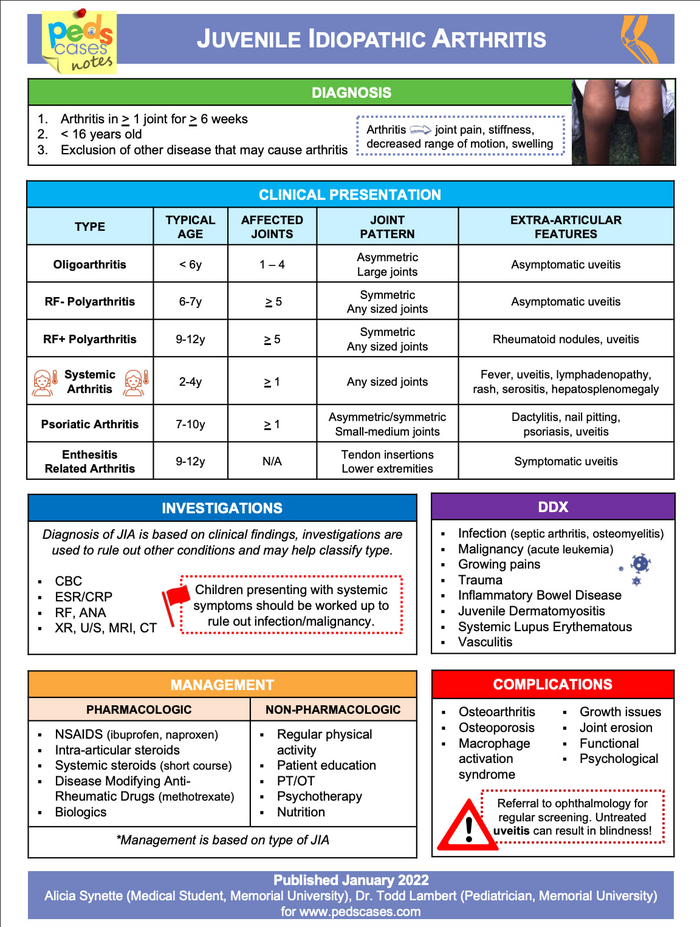
- Inflammatory (transient synovitis, juvenile idiopathic arthritis, reactive arthritis)
- Malignancy
- Pyomyositis
- Iliopsoas abscess
- Neurologic (stroke, ataxia)
- Gastrointestinal/GU (appendicitis, ovarian torsion, testicular torsion)
VITAMIN BCD (more expansive differential diagnosis for limp):
- Vascular: stroke, Legg-Calve-Perthes disease, avascular necrosis (such as in Sickle Cell disease)
- Infectious/Inflammatory: Septic arthritis, transient synovitis, osteomyelitis, Lyme arthritis, pyomyositis, iliopsoas abscess (such as in IBD), rheumatic fever, reactive arthritis
- Traumatic: Accidental or non-accidental trauma, toddler’s fracture
- Autoimmune: Juvenile idiopathic arthritis, reactive arthritis, acute rheumatic fever
- Metabolic: Scurvy, Ricket’s
- Iatrogenic/Idiopathic: Slipped capital-femoral epiphysis
- Neoplastic: bone tumors (Ewing sarcoma, osteosarcoma), leukemia, lymphoma
- Behavioral: diagnosis of exclusion
- Congenital: Developmental dysplasia of the hip, cerebral palsy
- Degenerative: less pertinent in pediatric population
Evaluation
Below are some tests that you may consider; use your history and physical exam to create an initial differential diagnosis to guide which tests to prioritize
Most Patients
Labs
- Complete Blood Count (CBC) for infectious and some oncologic etiologies
- Comprehensive Metabolic Panel (CMP)
- C- Reactive Protein (CRP) > Erythrocyte Sedimentation Rate (ESR)
- Creatine Kinase (CK), if concern for myositis
- Lyme testing, if rash or exposure history
- Blood culture
Imaging
- XR to assess for fracture or deformity, rule out primary bony oncologic diagnoses
- US joint to assess for effusion
- MRI joint to assess for effusion, osteomyelitis, myositis
If concerned for malignancy
- LDH, uric acid (if concerned for malignancy)
If concerned for inflammatory etiology
- UA (assess for urethritis in reactive arthritis – need non-catheterized specimen)
- Respiratory viral testing (transient synovitis)
- ANA panel (only if high suspicion for rheumatologic disorder)
- Anti-streptolysin O antibody, anti-DNAse B antibody (acute rheumatic fever)
- Stool cultures (reactive arthritis)
If history of restrictive diet
- Vitamin C level (scurvy)
- Vitamin D level (rickets)
If effusion is identified
- Synovial fluid studies – Cell counts, differential, culture, gram stain, Kingella PCR if < 5 years of age
- WBC > 50,000
- Concerning for septic arthritis
- High percentage of PMNs
- Positive gram stain or culture
- WBC 25,000-50,000
-
- Equivocal
- Consider Lyme arthritis or gonococcal arthritis
- WBC <25,000
-
- Transient synovitis
- Kocher Criteria: helpful to distinguish septic arthritis from transient synovitis.
Management of Common Causes of Pediatric Fever and Limp
- Transient synovitis
-
- Temporary inflammation of the lining of a joint space called the synovium thought to be related to immune response, often to viruses.
- Will often see bilateral effusions on hip US, differentiating this from septic arthritis which is typically unilateral.
- Typically self-resolves over a course of weeks.
- Recommend supportive care including NSAIDs and heat or ice packs for comfort.
- Osteomyelitis
-
- Common Pathogens: Staph aureus, Strep pyogenes, Kingella kingae (in children < 5 years)
-
- Treatment: Initiate empiric antimicrobials
-
-
- Cefazolin versus clindamycin if MRSA risk factors
- Narrow antimicrobials as tolerated based on culture data (if available) and transition to oral regimen if able
- Treatment duration varies based on clinical response and pathogen
-
- Septic arthritis
-
- Treatment: empiric antimicrobials
- Cefazolin versus clindamycin if MRSA risk factors
- Target pathogens: Staph aureus, Strep pyogenes, Kingella kingae (in children < 5 years)
- If synovial fluid culture positive for gram negative organism: ceftriaxone
- Narrow antimicrobials as tolerated based on culture data (if available) and transition to oral regimen if able
- Treatment duration varies based on clinical response and pathogen
- Treatment: empiric antimicrobials
- Limping in a pediatric patient has a very broad differential diagnosis, so it is important to have a framework to sort through the different categories of diagnoses and identify red flag diagnoses to rule out.
- History and physical exams are essential to narrowing down this broad differential diagnosis and guiding further consultation and workup.
- Understand the Kocher criteria for diagnosis of septic arthritis.
- Understand the interpretation of synovial fluid studies.
Click the drop down to reveal the correct answers
Q1: 4-year-old male presents with limp for the past day after 3 days of fever and cough, which has now resolved. Inflammatory markers are normal. On exam, pt refuses to bear weight on left leg and refuses to perform hip range of motion. What is the next step in imaging?
Q2: 10-year-old with history of recurrent fevers with rash, history of recurrent eye redness and pain presents to the ED for evaluation of fever and limp. What should be on your differential besides infection?
Answers
Q1: Ultrasound of left hip to evaluate for effusion
Q2: Juvenile Idiopathic Arthritis
- Articles
- The Limping Child | Pediatrics In Review | American Academy of Pediatrics (Access through biomedical library for full article)
- Pathway
- Other Resources

