Fever and Respiratory Distress
- Where to Find in the PSOM Curriculum
- Clinical Approach
- Differential Diagnosis
- Evaluation and Management
- Pearls
- Knowledge Check
- Resources
- Core 1 (Pre-clerkship)
- Microbiology and Infectious Diseases 1, Week 1: Properties of Bacteria, Bacterial Pathogenesis, Gram Positives Part 1 and 2,
- Microbiology and Infectious Diseases 1, Week 2: Respiratory Bacteria, Antibiotics
- Microbiology and Infectious Diseases 1, Week 5: Influenza Virus, Respiratory Bacteria
- Microbiology and Infectious Diseases 2, Week 1: Infection Syndromes; Organism, Cases, Antibiotics; Vaccines
- Integrative Systems, Pulmonology, Week 1: Hypoxemia; Lung Sounds; Pneumonia cases
- Integrative Systems, Pulmonology, Week 2: Bronchiolitis
- Core 2 (Clerkship)
- Pediatrics Clerkship didactics on Respiratory Distress
- Core 3 (Post Clerkship) Electives that may further knowledge
- Peds SubI, PEM, Peds PICU, Peds NICU, Peds ID, Peds Pulm
A 15-month-old presents with increased work of breathing and fever
History
- Preceding viral URI symptoms?
- Other associated symptoms and timeline? Fluctuation over course of the day?
- Duration and timing of fever?
- Have they had a history of wheezing or requiring albuterol?
- Apnea?
- Any sick contacts or exposures?
- What medications have they been given?
- Hydration?
- Exposure to allergens?
Physical Exam
- Assess overall appearance and mental status
- Vital signs
- Assess work of breathing (look for retractions, nasal flaring, grunting)
- Lung exam: Assess for wheezing, crackles, aeration, prolonged expiratory phase, cough, and symmetry
- Assess hydration status

The chart summarizes hallmark findings for five common pediatric respiratory conditions. Pneumonia and bronchiolitis are clinical diagnoses distinguished by focal lung findings versus viral symptoms in infants; asthma is suggested by a strong albuterol response and history of wheeze; pertussis features paroxysmal cough and requires confirmation; and croup presents with a barky cough, stridor, and nighttime worsening. The format helps quickly compare presentations when evaluating a child with cough or respiratory distress.
Bronchiolitis
- Etiology: viral infection
- Treatment: Supportive care
-
- Suctioning, hydration, nutrition, oxygen, fever management, respiratory support (High flow nasal cannula, non-invasive positive pressure, intubation)
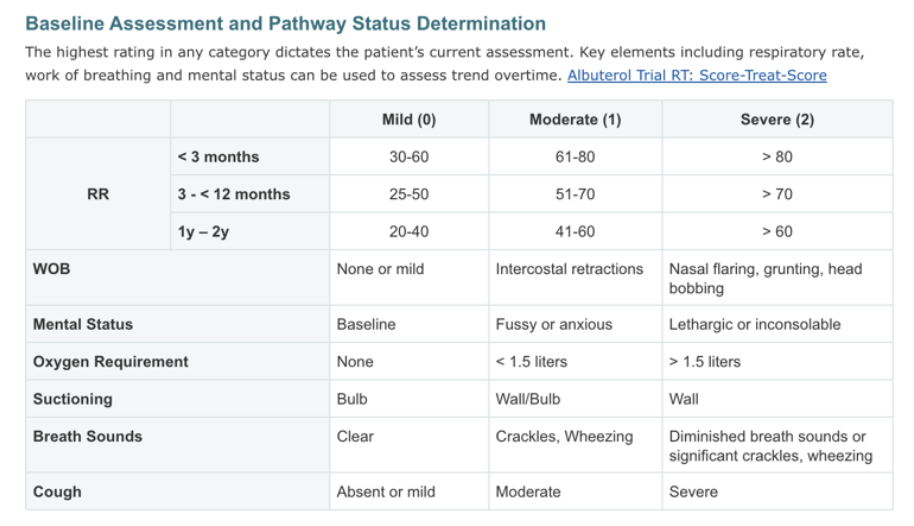
The table categorizes illness severity by assigning mild, moderate, or severe status depending on the highest abnormal finding. It compares respiratory rate cutoffs by age, escalating work of breathing from none to nasal flaring and grunting, mental status changes, oxygen requirements, suctioning needs, and progression from clear lung sounds to significant crackles or diminished breath sounds. This helps clinicians rapidly determine a child’s respiratory pathway and monitor for clinical changes over time.
Croup
- Etiology: parainfluenza specifically but many different viruses too
- Treatment
-
- Dexamethasone
-
- Inhaled racemic epinephrine
Pneumonia
- Etiology: viral infection, S. pneumoniae, S. aureus, M. pneumoniae, H. influenzae (if unvaccinated)
- Treatment options based on severity and age
-
- Mild: amoxicillin/ampicillin
-
- Moderate – Severe: Ceftriaxone, Clindamycin, Vancomycin
-
- Consider azithromycin in school-aged children for Mycoplasma pneumonia
-
-
- Colloquially called “Walking Pneumonia”
-
- Learn to differentiate sounds (see Pulmonary Module, Lung Sounds for review) of respiratory distress
- Suspect specific diagnoses based on age of presentation
- Croup and bronchiolitis tend to occur in infants and toddlers while asthma is more common in older/school-aged children
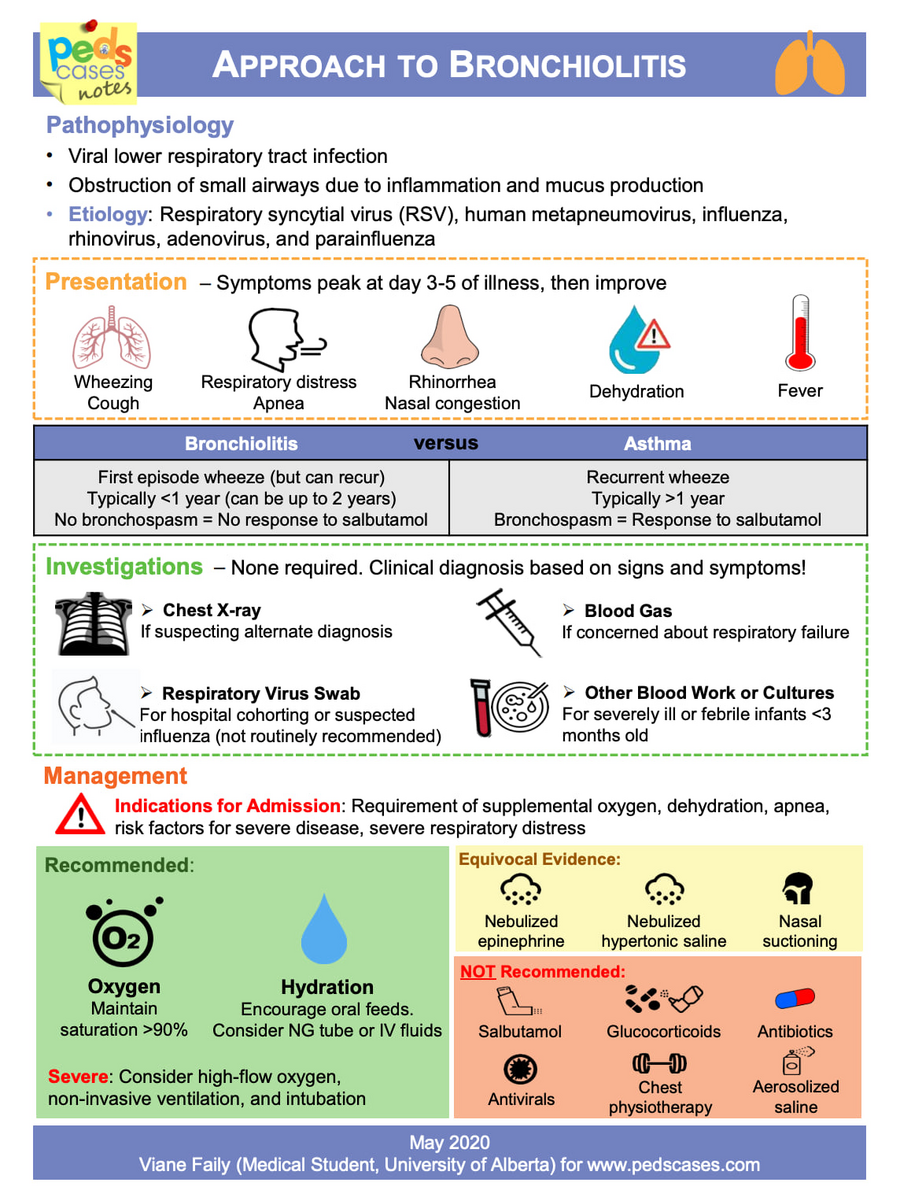
The chart explains that bronchiolitis is a viral lower respiratory infection causing airway inflammation and mucus obstruction, most commonly due to RSV. It highlights symptoms such as wheeze, respiratory distress, nasal congestion, dehydration, and fever, and outlines how bronchiolitis differs from asthma based on age and response to salbutamol. Management focuses on supportive care with oxygen and hydration, while tests and treatments such as routine X-rays, salbutamol, steroids, antibiotics, and antivirals are not recommended.
Click the drop down to reveal the correct answers
Q1: 9-month-old male presents with fever for 2 days and respiratory distress. On exam, he has copious nasal secretions with associated retractions that improve with nasal suctioning. What is the diagnosis?
Q2: 16-month-old female presents with fever for 1 day with respiratory distress. On exam, you notice a high pitched sound without your stethoscope on inspiration and expiration with inter-costal retractions. What is the treatment?
Q3: 15-year-old female presenting with cough, fever, and right-sided chest pain. On exam, you hear crackles over the right middle lobe. What is the most likely diagnosis?
Answers
Q1: Bronchiolitis
Q2: Racemic epinephrine: to address respiratory distress in the moment, Dexamethasone: to address ongoing airway inflammation and prevent recurrence of symptoms
Q3: Pneumonia
Videos
Podcasts
Pathways
Interactive Module
Articles

