Hypernatremia
A 9-month-old male is brought to the emergency department by his parents due to decreased oral intake and decreased wet diapers for the past two days.
He has had multiple episodes of non-bloody, non-bilious vomiting and several loose stools each day. His parents report he has been less active than usual and has had a dry mouth. They have been offering him diluted juice and Pedialyte at home but note he hasn’t been drinking much.
He was born full-term with no complications and is up to date on vaccinations. There is no travel history, sick contacts, or recent antibiotic use.
On exam, he appears lethargic. His weight is 7.4 kg (down from 8.2 kg at his 6-month visit). Temperature is 37.4°C (99.3°F), heart rate is 158/min, respiratory rate is 30/min, and blood pressure is 90/55 mmHg. He has dry mucous membranes, delayed capillary refill, and sunken eyes. His anterior fontanelle is sunken. No murmurs, hepatosplenomegaly, or rash are noted.
Initial labs:
- Na⁺: 158 mEq/L
-
K⁺: 4.2 mEq/L
-
Cl⁻: 115 mEq/L
-
HCO₃⁻: 20 mEq/L
-
BUN: 28 mg/dL
-
Cr: 0.6 mg/dL
-
Glucose: 92 mg/dL
Hypernatremia and Hyponatremia
- Hydration and fluid status does not exist in isolation: when your fluid status is abnormal, you run the risk of disrupting the electrolyte balance in your body too. One of the most significant electrolytes we worry about is sodium. In fact, serum sodium abnormalities are a reflection of water balance!
- 2 important terms
-
- Osmolality = concentration of solute (particles) dissolved in a solution
-
-
- Serum Osmolality in the human body = (1.8 * Na) + (Glucose /18) + (BUN / 2.8)
-
-
-
- Big take away = sodium has a big effect on serum osmolality!
-
-
- Tonicity = the affect a solution has on a cell based on movement of water
-
-
- Hypertonic solution: causes water to move out of a cell --> cell shrinks
-
-
-
- Hypotonic solution: causes water to move into a cell --> cell swells
-
- Sodium can be tricky – having low salt can be from being volume UP or volume DOWN... HUH? Let’s look into this more.
Hypernatremia
- Generally Na > 150 mEq/L in extracellular fluid (ECF)
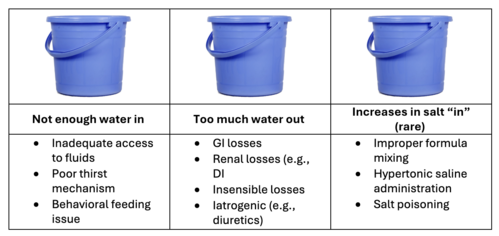
The image uses three identical blue buckets to illustrate the major mechanisms of hypernatremia. The first bucket lists causes of inadequate water intake, the second covers excessive water losses through GI, renal, insensible, or iatrogenic pathways, and the third highlights rare scenarios of increased salt administration. Together, the buckets emphasize a simple framework for understanding why serum sodium rises.
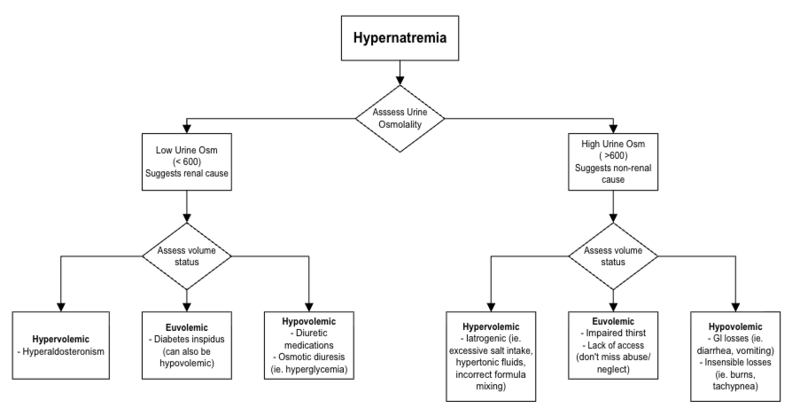
The diagram guides clinicians through the workup of hypernatremia by first assessing urine osmolality. Low urine osmolality suggests a renal cause such as diabetes insipidus, while high urine osmolality points toward non-renal etiologies like GI losses, insensible losses, or excessive salt intake. Volume status further categorizes patients as hypervolemic, euvolemic, or hypovolemic to refine the differential diagnosis.
Identifying cause
- Check urine osmolality to differentiate renal and non-renal causes
- Assess volume status
- Can also check urine Na
Management
- Correct Sodium slowly! Calculate and gradually replace free water deficit
- If you correct hypernatremia too fast, you can cause cerebral edema
- “High to Low your brains will blow”

