Infant Nutrition
Key Conditions/Topics
- Normal infant weight gain
- Formula
- Failure to Thrive/Growth Faltering
- Core 1 (Pre-Clerkship)
- Biochemistry – Glycolysis, Met Round 1
- Genetics – Cystic Fibrosis
- Cell, Tissue, and Biology - Lab 5: Cartilage and Bone Pre-work; Co and Counter-Transport (CF)
- Anatomy and Imaging -
- The Alimentary Tract and GI Circulation
- Heart (Congenital heart disease)
- Microbiology II - Parasites
- Immunology – Immunodeficiencies
- Endocrine – Growth and puberty; Calcium metabolism
- Gastroenterology – Nutrition, wellness and health; Nutrition and obesity
- Cardiology – Congenital heart disease
- Pulmonary – Pediatric Pulm
- Core 2 (Clerkship)
- Pediatrics Clerkship Growth and Nutrition lecture
- Core 3 (Post Clerkship) Electives that may further knowledge
- NICU elective
Term Infant Weight Gain
|
Age |
Calories (kcal/kg of body weight) |
Mean Weight Gain |
|
0–3 mo |
90-135 |
~ 25-30 g/d |
|
3–6 mo |
80 |
~ 15-20 g/d |
|
6–12 mo |
80 |
~ 10-15 g/d |
Considerations for the Term Infant
Many newborn infants lose up to 10% of their birth weight within the first week of life due to fluid losses. Newborns will usually regain their birth weight within 7 days and are expected to have regained it by 14 days. A health term infant should double their birth weight by 5–6 months of age.
To prevent rickets, intake of 400 IU per day of Vitamin D3 is recommended for all infants who are exclusively breastfed or receiving <32 oz of formula per day.
References:
"Nutrition in Infancy", The Clinician’s Guide to Pediatric Nutrition, Natalie D. Muth, MD, MPH, RDN, FACSM, FAAP, Mary Tanaka, MD, MS, FAAP
Preterm Infant Weight Gain
Generally, intake of 110 to 130 kcal/kg/day is needed for satisfactory preterm infant growth. More calories may be needed if growth is not adequate. Certain conditions that accompany prematurity may result in increased energy requirements such cardiac conditions or chronic lung disease, thus necessitating a degree of individualization.
Most formula-fed late preterm infants are fed a 19−20 kcal/oz term infant formula, those who are small for gestational age (<2,000 g) or who exhibit excessive weight loss or poor weight gain (<15 g/day) may require higher-calorie full-term or post discharge preterm infant formula. Many preterm infants may benefit from supplementation with 22 kcal/oz premature formula for the first few months if they are slow to gain weight. Most infants born at greater than 34 weeks' gestation only require caloric fortification for 1 to 2 months, or until they are able to take larger volumes of breastmilk to provide the additional calories needed.
The American Academy of Pediatrics (AAP) recommends a weight gain of 20-30 g/day in preterm infants, especially those over 2 kg, to help them catch up on growth. This can also be expressed as a weight gain velocity of 15 g/kg/day, which is a commonly used goal in the NICU. There is some debate about the recommended weight gain goal, with some studies suggesting that a weight gain velocity of 20-30 g/kg/day may be necessary for optimal long-term neurodevelopmental outcomes.
Consider transitioning from higher-calorie formula to standard 19−20 cal/oz infant formula when the infant is demonstrating good weight gain (30 to 40 g/day) and growth is above the 10th percentile for postmenstrual age on the World Health Organization Growth Charts for Infants 0 to 24 Months.
Considerations for the Preterm Infant
- Avoid soy protein-based formula for preterm infants because of the increased risk of osteopenia due to inadequate calcium/phosphorous content.
- After 2 weeks of age, preterm infants not being fed an iron-fortified formula should receive a source of iron providing 2 to 4 mg/kg/day, often until 6 to 12 months of age (depending on diet). Iron stores can be assessed routinely, and iron supplementation adjusted accordingly.
References:
Mandy Brown Belfort, Sara E. Ramel; NICU Diet, Physical Growth and Nutrient Accretion, and Preterm Infant Brain Development. Neoreviews July 2019; 20 (7): e385–e396.
Jennifer AF Tender; Preterm Infant Nutrition. Pediatr Rev September 2004; 25 (9): 328–329.
"Nutritional Needs of the Preterm Infant", Pediatric Nutrition, American Academy of Pediatrics, Frank R. Greer, MD, FAAP, Steven A. Abrams, MD, FAAP
Forms of Nutrition
Enteral: Term Infant Formula (12 months of younger)
Regular infant formulas are intended for healthy, full-term infants. These formulas may contain:
- Cow’s milk: Ex. Enfamil, Similac
- Goat’s milk: Ex. Kabrita, Kendamil goat
- Soy Milk
- Indications: Congenital lactase deficiency, galactosemia
- Examples: Similac Soy Isomil, Enfamil Prosobee
There are different classes of formula made to address specific clinical scenarios:
- Partially hydrolyzed infant formula: Formula that contains cow’s milk proteins that have already been partially hydrolyzed, or broken down, and may be easier to digest.
- Indications: In 2008, updated AAP recommendations stated that for infants at high risk of developing atopic disease who are not breastfed exclusively for 4 to 6 months or are formula-fed, there is evidence that atopic dermatitis may be delayed or prevented by the use of partially hydrolyzed formula compared with cow milk-based formula.
- Examples: Enfamil NeuroPro Gentlease, Gerber Good Start Gentle, Similac Pro-Total Comfort
- Spit-up formulas are thickened with rice starch
- Indications: Gastroesophageal Reflux
- Ex. Enfamil AR, Similac Sensitive RS
Specialty formulas are intended for use by an infant who has an inborn error of metabolism, low birth weight, or other medical or dietary problems.
- Hypoallergenic formulas are defined by the American Academy of Pediatrics (AAP) as “formulas [that] demonstrate that they do not provoke reactions in 90% of infants or children with confirmed cow milk allergy with 95% confidence when given in prospective randomized, double-blind, placebo-controlled trials.” This qualifies extensively hydrolyzed and free amino acid-based formulas as hypoallergenic.
- Indications: Milk protein allergy, possibly short gut syndrome
- Examples of extensively hydrolyzed formulas: Similac Alimentum, Enfamil Pregestimil
- Examples of Amino Acid based formulas: Elecare, Neocate, Nutramigen AA
How to Use:
Standard formula mixing is 2 fluid oz of water with 1 unpacked level scoop of formula (measure water first and add scoops to water) to make 2 oz of formula. Giving an infant <6 months old any other fluids or incorrectly mixed formula risks electrolyte imbalances. There are three formulations:
- Powder — Must be mixed with water before feeding as above.
- Liquid concentrate — Must be mixed with an equal amount of water before feeding.
- Ready-to-feed — Requires no mixing.
References:
- Andres Martinez, Martha P. Ballew; Infant Formulas. Pediatr Rev May 2011; 32 (5): 179–189.
O'CONNOR, N. R. (2009). Infant formula. American family physician, 79(7), 565-570.
https://www.fda.gov/food/resources-you-food/infant-formula
Tube Feeds:
Tube feeding (TF) is a mode of providing enteral nutrition when oral feeding is not possible or not sufficient. TF is delivered through a medical device that can be placed into the stomach, duodenum, or jejunum via either the nose, mouth, or the percutaneous route. Below is a chart of tube feed formulas modified from the AAP for children > 1 year of age. Free water needs will need to be addressed via continuous free water or flushes.
|
Formula Category |
Indications |
Examples |
Comments |
|
Standard Pediatric Enteral Formulas |
Normal GI tract requiring a complete or supplemental source of energy from tube feeding |
Boost Kid Essentials, Compleat Pediatric, |
|
|
Calorie-dense Pediatric Formulas |
Normal GI tract requiring increased energy needs, shortened feeding schedules, fluid restriction, or have volume intolerance |
Children 1-13 years: |
|
|
Reduced-calorie Pediatric Enteral Formulas |
Age 1-13 years with decreased energy needs requiring a lower-energy complete feeding |
Compleat Pediatric Reduced Calorie, PediaSure SideKicks 0.63 kal/mL |
|
|
Hydrolyzed Pediatric Formulas |
Impaired GI tract function requiring peptide-based complete nutrition formula; may be beneficial for use in malabsorption, short bowel syndrome, chronic diarrhea, delayed gastric emptying, or for previous intolerance issues with intact protein formulas |
PediaSure Peptide 1.0, |
|
|
Free Amino Acid Pediatric Formulas |
For children with impaired GI tract function requiring a hypoallergenic, amino acid-based formula; may be beneficial for use in patients with multiple food allergies, eosinophilic GI disorders, malabsorptive conditions, short bowel syndrome, and other GI tract impairments |
Alfamino Junior, Elecare Junior, Neocate Junior, Neocate Splash, Vivonex Pediatric |
|
Some formulas may use porcine enzymes to hydrolyze the proteins, and, therefore, these formulas are not considered halal or kosher. Information about Halal and Kosher certification can be found online and on many of the formula labels. For example, Similac Sensitive and Gerber Good Start Soy are both Kosher and Halal.
References:
Aamer Imdad, Rida Sherwani, Kellie Wall; Pediatric Formulas: An Update. Pediatr Rev July 2024; 45 (7): 394–405.
Sarita Singhal, Susan S. Baker, Georgina A. Bojczuk, Robert D. Baker; Tube Feeding in Children. Pediatr Rev January 2017; 38 (1): 23–34.
A 15-month-old male presents to your primary care practice for a follow up visit. His parents are concerned about her growth, noting that his birth weight was in the 50th percentile. Her weight fell to the 30th percentile at his 6-month visit and is now in the 10th percentile. Both his head circumference and length have remained in the 30th percentile since birth.
- Birth history, birth weight, and prenatal care, social support at home
- Feeding history is the most important part!
- Walk through how they are mixing formula
- How many scoops of formula to water? Do you put water in first or the powder first? How many bottles do you prepare in a day? How many ounces per bottle? Who mixes the bottles?
- Frequency, length, number per day, longest interval between feedings
- If breast/chestfeeding, ask about issues with latching, frequency, pumping. Are they supplementing? Are they feeding on one or both breasts. Ask about the use of nipple shield
- Address access to formula and any concerns for food insecurity
- Walk through how they are mixing formula
- Once you've determined caloric intake the next questions are surrounding oropharyngeal function:
- Ask about coughing, choking gagging, spitting up, vomiting
- Arching (concerning for GERD), discomfort, respiratory symptoms with feeds
- Ask about elimination
- What is the number of wet diapers and stool diapers per 24 hours
- Stool appearance (consistency, color)
- Presence of orange or red crystal/powder in diaper
- Presence of blood or mucus in stool
- What is the number of wet diapers and stool diapers per 24 hours
- Focused additional history:
- Cardiac disease: Is there sweating during feeds, belly distension (hepatomegaly), cyanosis
- Neurologic: Have you noticed loss of milestones, poor tone, poor suck
- Abdominal/Malabsorption: Diaper dermatitis, profuse vomiting
- Immunodeficiency: Frequent infections
|
General |
|
|
HEENT |
|
|
Resp |
|
|
Cardiac |
|
|
GI |
|
|
Skin |
|
|
Neuro |
|
Source: Snellgrove S, Molina A, Lee N, Masur S, Chiu C, Berk J. #39: Failure to Thrive – Growing into Focused Management. The Cribsiders Pediatric Podcast. November 24, 2021.
1. Does this meet criteria for growth faltering?
Yes. Infants who fall below weight-for-age or weight-for-length percentile or whose rate of weight gain declines across 2 major percentiles (ie, 90th, 75th, 25th) should be assessed for growth faltering.
2. What is the first step in evaluating an infant with growth faltering concerns? The history! See above
3. How is the pattern of growth faltering (i.e. length, weight, head circumference) helpful?
Inadequate calorie intake is the most common cause of growth faltering and should occur in the following pattern: weight → height → head circumference. If the growth faltering does NOT spare head circumference, there should be higher suspicion for an underlying cause such as metabolic disorder, TORCH infection, antenatal ischemic insult/stroke, or neuro-anatomic abnormalities. Endocrine disorders may affect only length while weight continues to follow its curve.
4. When are labs indicated?
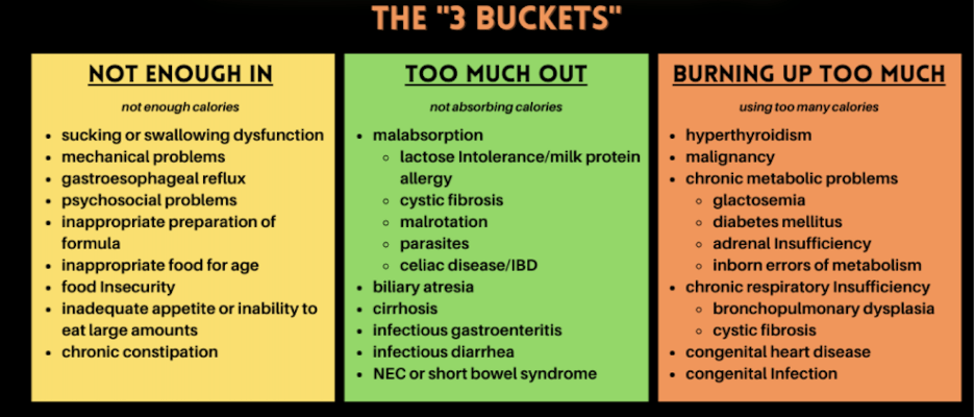
Labs are rarely indicated unless you are concerned about “too much out” or “burning up too much” categories guided by clinical suspicion. Additionally, if initial intervention fails, you could consider additional evaluation. If the patient is having abnormal stools, consider initial malabsorption workup. Other etiologies will likely require other specific testing (CXR, echo, sweat test, etc.) and consultation with the respective specialty. If developmental or cognitive delay is identified, genetic work should also be considered.
Pearls
- Consider alternate formulas based on medical indication
- Use extensively hydrolyzed or amino acid-based formulas for infants with confirmed cow’s milk protein allergy.
- Partially hydrolyzed formulas may help prevent atopic dermatitis in at-risk infants
- Evaluate Failure to Thrive (Growth Faltering) Systematically:
- Start with feeding history and formula preparation.
- Consider 3 categories: not enough in, too much out, or burning up too much
- Podcasts:
- Snellgrove S, Molina A, Lee N, Masur S, Chiu C, Berk J. “#39: Failure to Thrive – Growing into Focused Management”. The Cribsiders Pediatric Podcast. https:/www.thecribsiders.com/ Nov 24, 2021
- Nutrition Advice for Premature Babies at Discharge from the NICU - CHOP OPEN
- Infant Nutrition: Are Your Newborn and Infant Patients Getting Enough Vitamin D and Iron? - CHOP OPEN
- AAP Growth Faltering in Newborns and Infants
- Pathways: https://pathways.chop.edu/clinical-pathway/infant-malnutrition-ftt-clinical-pathway
Click the drop down to reveal the correct answers
Q1: A 1-month-old infant presents for a routine visit. His mother reports that he is exclusively breastfed. He is growing well and has no medical problems. Which of the following is the most appropriate recommendation regarding supplementation?
A) No supplementation is needed as he is breastfeeding well
B) Begin iron supplementation
C) Begin 400 IU of vitamin D3 daily
D) Switch to formula to meet vitamin D and iron needs
Q2: A 3-month-old infant is brought to the clinic with a 2-week history of persistent diarrhea, blood-streaked stools, and decreasing weight percentiles. He is transitioning from pumped breast milk to cow’s milk-based formula. He was recently switched from one cow's milk-based formula to another without improvement. On exam, he appears fussy but well hydrated. The pediatrician suspects a cow’s milk protein allergy.
Which of the following is the most appropriate next step in formula management for this infant?
A) Switch to a soy-based formula
B) Transition to goat’s milk formula
C) Begin an extensively hydrolyzed formula
E) Use a thickened, rice-starch formula for reflux
Q3: A 4-month-old infant is brought in for evaluation of poor weight gain. The child was born full-term with a birth weight at the 50th percentile, but his weight is now below the 5th percentile while his length and head circumference remain around the 25th percentile. The parent reports that feeding sessions are difficult—the infant arches his back, cries during and after feeds, and often spits up large volumes of milk. The baby feeds every 2–3 hours but appears irritable and gassy. There are no signs of diarrhea, and the infant is otherwise alert and developmentally appropriate.
Which of the following is the most likely contributor to this infant’s failure to thrive?
A) Inadequate formula mixing
B) Gastroesophageal reflux disease (GERD)
C) Congenital heart disease
D) Cow’s milk protein allergy
E) Hypothyroidism
Answers:
Q1: C) Begin 400 IU of vitamin D3 daily
Rationale: Exclusively breastfed infants and formula-fed infants consuming less than 32oz daily of formula should receive 400 IU of vitamin D3 daily. AAP recommends starting iron supplementation at 4 months of age for exclusively or mostly breastfed infants until iron-rich complementary foods are introduced
Q2: C) Begin an extensively hydrolyzed formula
Rationale: Extensively hydrolyzed formula or amino acid-based formula are less likely to trigger allergic response. There is some cross-reactivity with soy-based and goat’s milk formula in infants with cow’s milk protein allergy.
Q3: B) Gastroesophageal reflux disease (GERD)
Rationale: The patient exhibits symptoms of GERD including back-arching, large-volume spit-ups, and crying during feeds.

