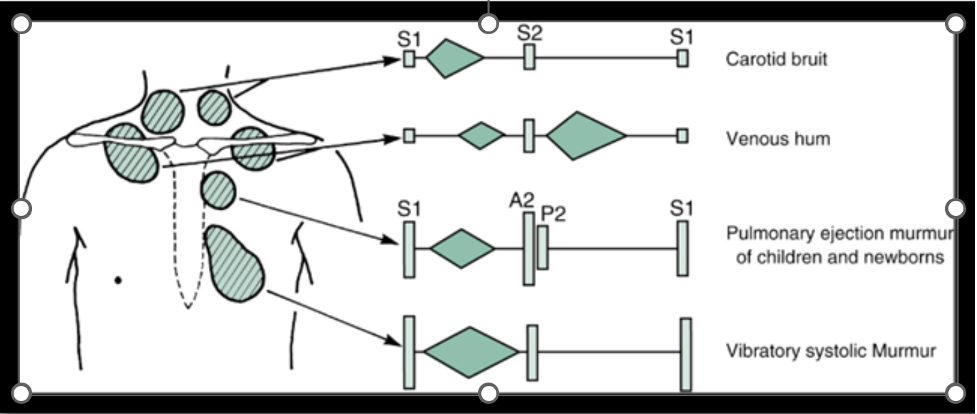
Innocent Murmurs
Approach to the Auscultation of Murmurs
Park's Pediatric Cardiology for Practitioners. Park, Myung K., MD, FAAP, FACC; Salamat, Mehrdad, MD, FAAP, FACC. Published December 31, 2020. Pages 6-30. © 2021
Very common benign murmur heard at the lower left sternal border and apex. Low pitched, mid systolic murmur, described as musical or vibratory in quality (think twanging of a guitar string). Will decrease in intensity with standing up or Valsalva maneuver. Can be accentuated by fever, anemia or exercise.
Soft, low pitched, continuous murmur heart at the high right sternal border and infraclavicular area from turbulent flow at the connection between the jugular vein and superior vena cava. This murmur is accentuated by sitting and will disappear when supine or with rotating the head to the right or compression over the right jugular vein.
Blowing, medium pitched, systolic ejection murmur heard at the left upper sternal border and may transmit to the back. Most frequently heard in adolescents. Represents normal vibrations heard in the pulmonary trunk with ejection. Should be associated with a normal S2 (to distinguish from pulmonary stenosis or an atrial septal defect). Will soften with standing or Valsalva.
Short, systolic ejection murmur heard at the left upper sternal border with radiation to bilateral axillae and back. Occurs exclusively in newborns secondary to relative hypoplasia of the pulmonary artery branches that causes flow acceleration at the branch points. In fetal circulation, only 15% of the combined ventricular output travels through the branch pulmonary arteries (majority of venous inflow travels across the foramen ovale or ductus arteriosus). This causes relative hypoplasia of the branch pulmonary arteries. After birth, with normal blood flow and growth, this resolves in the first few months of life. If persists, a structural narrowing of the pulmonary vessels should be suspected.

