Intussusception
- Where to Find in the PSOM Curriculum
- Clinical Approach
- Evaluation and Management
- Pearls
- Knowledge Check
- Resources
- Core 1 (Pre-Clerkship)
- Biomedical Science
- Anatomy and Imaging
- The Alimentary Tract and GI Circulation
- Anatomy and Imaging
- Biomedical Science
- Core 2 (Clerkship)
- Pediatric Clerkship didactics - Acutely Ill Child
- Core 3 (Post Clerkship) Electives that may further knowledge - Peds EM, Peds Surgery
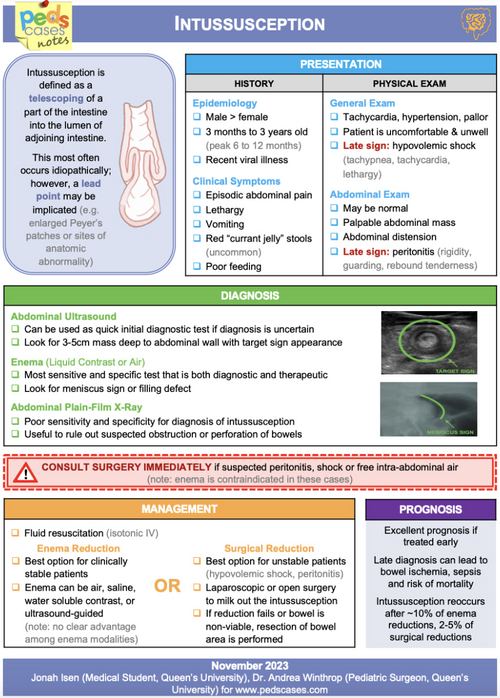
- Classic presentation: Classic triad of pain, palpable sausage-shaped abdominal mass, and currant jelly stool (seen in <15% of patients)
-
- Pain is typically intermittent, severe, crampy, and progressive (15-20 minute intervals
-
- “Currant jelly” bloody stools occur in <25% of cases – typically a late symptom indicative of necrosis
-
- Scaphoid/empty right lower quadrant may be present (Dance sign)
- Atypical presentation: Can present without pain or without bloody stools. Occasionally, presenting symptoms is just lethargy or altered consciousness without pain or rectal bleeding. Thus, intussusception should be considered in the evaluation of otherwise unexplained lethargy or altered consciousness, especially in infants.
Evaluation
- Ultrasound is primary test for diagnosis (negative predictive value is ~100%)
- Classic "target sign" appearance, usually located in the right lower quadrant (ileo-cecal region)
- Two-view abdominal radiograph is often done to rule out perforation, especially prior to reduction
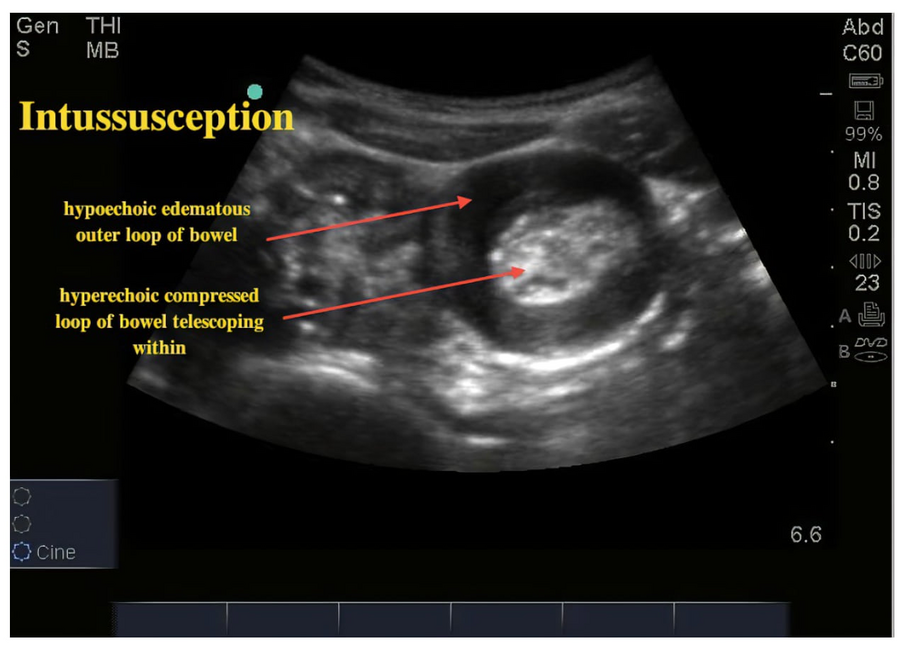
Source: Ultrasound Cases
- Stabilize the patient – IVF/labs if evidence of volume depletion or shock
- Once ultrasound confirms ileo-colonic intussusception, as long as there is no evidence of perforation and hemodynamically stable, attempt nonoperative reduction in radiology using saline/contrast or air enema (success rate 70-85% and 80-95% respectively at CHOP)
-
- Lower chance of successful reduction: <1yo (especially <3mo), >5yo (greater risk of pathologic lead point), hematochezia, longer duration of symptoms, xray findings of obstruction.
-
- If progressive movement of intussusception and hemodynamically stable, may have success from delayed repeat enema (50% success)
- If reduction is completely unsuccessful, if unable to reduce after multiple attempts, hemodynamically unstable, or evidence of perforation, will need surgical reduction/intervention
NOTE: Small bowel-small bowel intussusception is more likely to resolve spontaneously especially if short in length (<2.3cm). Consider observation and repeat imaging for resolution if symptoms are mild or if asymptomatic. Enema reduction is less likely to be successful, but can be attempted. Surgical reduction is needed if continued symptoms and not spontaneously reducing (one study showed an average length of 7.3 cm in children requiring surgical intervention.
- If reduction is uncomplicated, can consider trial of PO clears 2 hours after reduction and discharge 4 hours after reduction
- Admission for observation should be considered in ages <6 months old or >36 months old or if there are continued symptoms after reduction
- Approximately 10% of patients experience recurrence with 4% of patients having a recurrence within 48 hours. Therefore, anticipatory guidance should be given and there should be a reliable plan for follow-up and return to care with symptom recurrence.
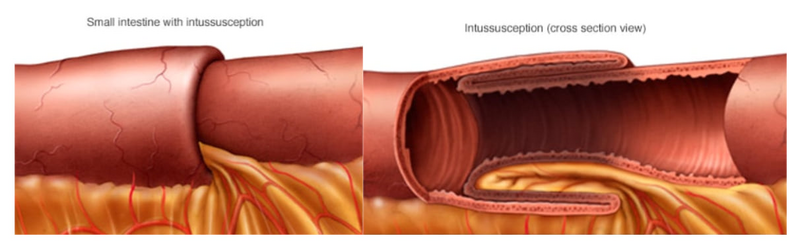
- When the bowel telescopes onto itself dragging the mesentery with it. The trapping of the mesentery causes venous and lymphatic congestion that ultimately can lead to ischemia, perforation, and peritonitis.
- Most commonly occurs at the ileocecal junction (90% of cases), but can also occur in the small bowel alone
- Peak incidence is between 4 and 36 months of age, and it is the most common cause of intestinal obstruction in this age group
- Important to consider this diagnosis in children outside this age range. Approximately 10 percent of cases are in children over five years, and 3 to 4 percent in those over 10 years
- Consider intussusception in younger kids presenting with lethargy
- Diagnosed with ultrasound
- Ileo-colonic intussusception usually needs to be reduced by air/contrast/saline enema whereas small bowel-small bowel intussusception usually spontaneously reduces.
- Majority of cases are idiopathic without a clear diagnosis or trigger, but it can also be due to a trigger such as infection (30% of patients have infectious symptoms) or pathologic lead point (25% of cases)
|
Pathologic Lead Points |
|
|
Bowel Edema/Inflammation |
Bowel Lesions/Mass |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Peds Cases Summary of Intussusception
Click the drop down to reveal the correct answers
Q1. What is the peak age range for intussusception in children?
Q2. What is the most common location for intussusception to occur in children?
Q3. How is intussusception diagnosed?
Q4. How is intussusception treated?
Q5. What age groups are at higher risk of non-successful reduction with enemas?
Q6. What is the recurrence rate for intussusception after successful reduction?
Q7. Infants with intussusception can present with what atypical symptom?
Q8. A 2-year-old with abdominal pain presents to the emergency department and has a “target sign” on imaging. What is the diagnosis?
Q9. What is the treatment for small bowel-small bowel intussusception?
Q10. After successful reduction of intussusception, when can PO trial of clears be done? When can the patient discharge?
Answers
Q1. The peak incidence of intussusception occurs between 4 and 36 months of age.
Q2. The majority of intussusception cases occur at the ileocecal junction, accounting for 90% of cases.
Q3. Diagnosis is made by ultrasound, which typically shows the “target sign” in the right lower quadrant. A two-view abdominal radiograph is often obtained beforehand to rule out perforation.
Q4. Intussusception is treated with a contrast/saline or air enema.
Q5. Higher risk of non-successful reduction is seen in:
- Infants <1 year (especially <3 months)
- Children >5 years (increased risk of pathologic lead points)
Q6. Approximately 10% of patients experience recurrence after successful reduction. About 4% of recurrences happen within 48 hours. Anticipatory guidance should be given at discharge.
Q7. Lethargy or altered mental status. Intussusception can present with lethargy as the only symptom, without pain or rectal bleeding—especially in infants.
Q8. Intussusception. The “target sign” on ultrasound confirms the diagnosis.
Q9. Observation with repeat imaging is preferred if symptoms are mild or absent. Small bowel-small bowel intussusception often resolves spontaneously if short (<2.3 cm). Enema is less likely to help but can be attempted. Surgery is required if symptoms persist or the intussusception is long (e.g., >7 cm).
Q10. If the reduction is uncomplicated:
- A trial of PO clears can begin 2 hours after reduction
- Discharge is typically safe 4 hours post-reduction

