Pathologic Murmurs
Innocent and Pathologic Murmurs by Auscultation Location
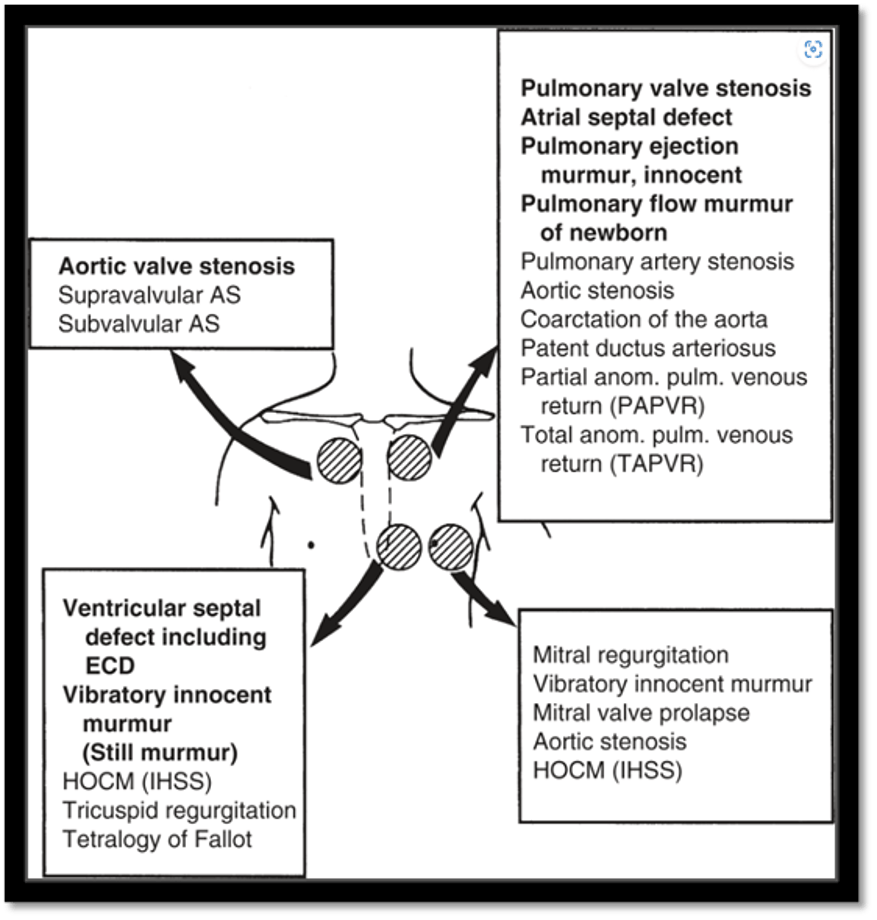
Park's The Pediatric Cardiology Handbook. Park, Myung K., MD, FAAP, FAAC; Salamat, Mehrdad, MD, FAAP, FACC. Published December 31, 2021. Pages 3-37. © 2022. Fig. 1.7
- Heart defects are the most common birth defect and occur in 8/1000 live births. This does not include bicuspid aortic valves which occur in 2-3% of the population but as the valve function is typically normal classically do not cause hemodynamic issues or changes to the cardiac exam until the later decades of life.
- The most common congenital heart defect in childhood is ventricular septal defects (comprising ~40% of congenital heart disease). Other common defects are atrial septal defects, patent ductus arteriosus and valvar pulmonary stenosis.
- Critical congenital heart disease is a grouping of congenital heart defects that are present at birth and require early surgical or catheter based intervention in order for the neonate to survive. Most (but not all) of these defects are “ductal dependent” and require the PDA to sustain either systemic or pulmonary circulation. About 25% of heart defects are critical. Examples of these defects are hypoplastic left heart syndrome, transposition of the great arteries, critical aortic or pulmonary stenosis, critical aortic coarctation, pulmonary atresia and/or tricuspid atresia.
- Not all neonates with congenital heart disease will have a murmur. Pathologic murmurs are caused by flow acceleration (turbulent flow) going across narrowed vasculature/obstructed valves, leakage (regurgitation) of valves or by flow crossing holes between the ventricles. All aspects of the exam are important in investigating an infant for possible congenital heart disease. This includes vital signs that include blood pressures of all extremities and saturations in upper and lower extremities, respiratory exam, abdominal (liver) exam, and a careful examination of the pulses and perfusion.
Common Congenital Heart Defects
- Acyanotic Congenital Heart Disease
- Shunt Lesions
- Ventricular Septal Defect
- Atrial Septal Defect
- Endocardial Cushion Defect/AV canal defect
- Patent Ductus Arteriosus
- Obstructive Lesions
- Aortic or Pulmonary Stenosis
- Coarctation of the Aorta
- Shunt Lesions
- Cyanotic Congenital Heart Disease
- 5 “T’s”
- Transposition of the Great Arteries
- Tetralogy of Fallot
- Tricuspid Atresia
- Total Anomalous Pulmonary Venous Return
- Truncus Arteriosus
- 5 “T’s”
- Most common inherited cardiac disease with a prevalence estimated at 1/500 it typically results from a genetic mutation in the proteins of the cardiac sarcomere and is inherited in an autosomal dominant pattern. While the penetration is variable, it can result in a progressive thickening of the left ventricle that results in potential obstruction of the left ventricular outflow tract. It is suspected in the presence of left ventricular hypertrophy without dilation and in the absence of another causative condition (systemic hypertension, aortic valve disease, etc…). In addition to possible outflow tract obstruction, hypertrophic cardiomyopathy can cause lethal arrhythmias, diastolic dysfunction and myocardial ischemia. Undiagnosed hypertrophic cardiomyopathy is the most common cause of sudden cardiac death in athletes in the United States.
- While typically presenting in adulthood, it can present in older childhood. Earlier presentations of hypertrophic cardiomyopathy are highly associated with genetic or metabolic syndromes (for example Noonan’s syndrome). In the presence of outflow tract obstruction, hypertrophic cardiomyopathy will cause a systolic ejection murmur over the LV outflow tract (left sternal border). This murmur will classically get louder when standing or with the Valsalva maneuver (an important distinguishing feature from the more common innocent Still’s or pulmonary flow murmurs seen in childhood). It will soften when supine or squatting. EKG abnormalities are also frequently seen in hypertrophic cardiomyopathy (left ventricular hypertrophy, ST or T wave abnormalities).

