Prolonged Fevers
- Where to find in the PSOM Curriculum
- Clinical Approach
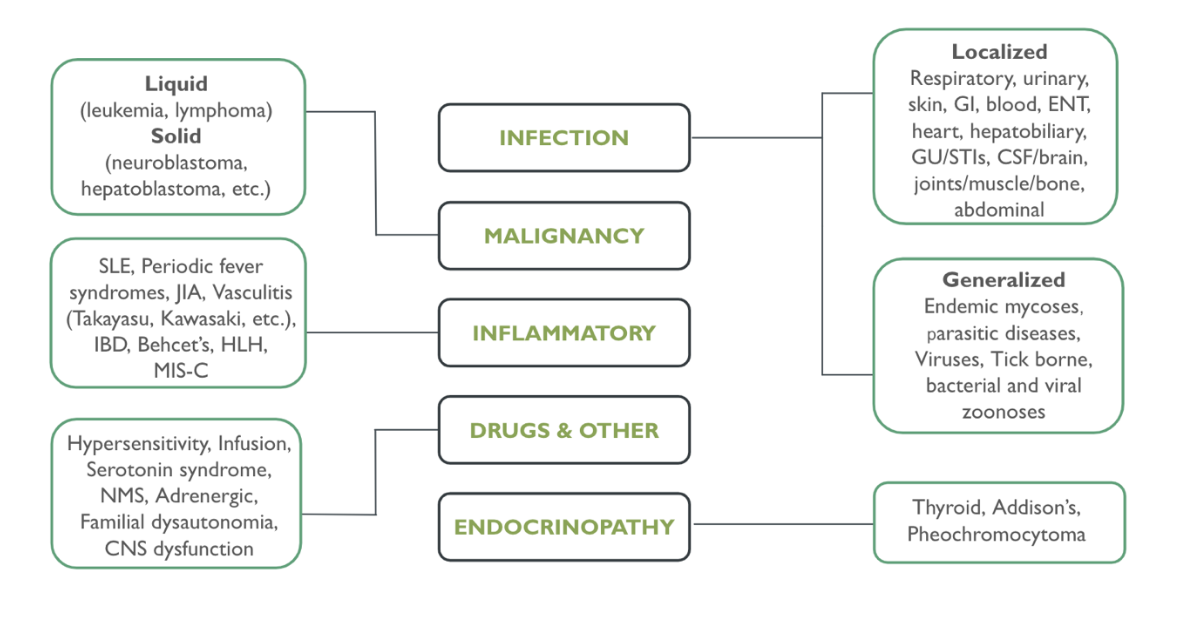
- Differential Diagnosis
- Evaluation and Management
- Pearls
- Knowledge Check
- Resources
- Core 1
- Integrative Systems, MDTI: SLE
- Integrative Systems, Dermatology, Week 1; Pediatric Dermatology (Kawasaki)
- Integrative Systems, MDTI: Acute Leukemia
- Core 2
- Pediatrics Clerkship didactics on Fever
- Core 3 (Electives that may further your knowledge)
- Peds SubI, PEM, Peds PICU, Peds ID, Peds Rheum, Peds Onco
6-year-old with 2 weeks of recurrent fevers
History
- Immunization history, Medication history
- Travel History, exposure to animals, tick-bites
- Pattern and timing of fevers, whether they have been occurring daily
- Sexual History
- Other associated symptoms including muscle/joint stiffness or pain, oral/aphthous ulcers, lymphadenopathy, rashes, sore throat, extremity swelling, ear pain, conjunctivitis or mucous membrane changes
- B symptoms – unintentional weight loss, hepatosplenomegaly, night sweats
- Family history – cancer, autoimmune conditions
Physical Exam
- Skin exam (look for rashes)
- Joint exam
- Lymphadenopathy?
- Cardiac exam (murmur/friction rub) – pericarditis?
- Pulmonary exam and work of breathing
- ENT (TM, pharyngitis)
- Abdominal exam (mass, tenderness, hepatosplenomegaly)
General: CBC with diff, CMP, UA, blood cultures, CXR, ESR, CRP, LDH, CPK, CMV/EBV, adenovirus, consider other tests as indicated
Rheumatologic/Immunologic
- Systemic Lupus Erythematosus (SLE)
- Signs/Symptoms: Malar rash, discoid rash, photosensitivity, oral ulcers, arthritis, fatigue, weight loss, alopecia, lymphadenopathy, CNS features
- Laboratory Tests: Autoantibodies (ANA, anti-dsDNA, Anti-Smith antibodies, Anti-Ro/La), Complement (low C3 and C4), CMP – Cr/BUN for kidney involvement, CBC – hemolytic anemia (hgb<12), thrombocytopenia (<150k), leukopenia (WBC <4k), lymphopenia (lymphocytes < 1500), UA (hematuria, proteinuria), Elevated ESR (with normal CRP)
- Imaging: Echo, CXR – serositis
- Management: Steroids, immunosuppression
- Systemic Juvenile Arthritis (JIA)
- Signs/Symptoms: Arthritis 6+ weeks, rash, lymphadenopathy, hepatosplenomegaly
- Incidental findings -> Echo: pericardial effusion may be noted, CXR- pleural effusion
- Laboratory Tests: CBC (leukocytosis, thrombocytosis), elevated ESR & CRP, evaluation for MAS (ferritin, d-dimer), CMP (hypoalbuminemia, elevated AST/ALT), immune activation (elevated S100A8/A9 and S100A12, IL18), NEGATIVE RF and ANA
- Management: NSAID, immunosuppression/immunomodulation
Inflammatory Bowel Disease (IBD)
- Signs/Symptoms: Diarrhea/bloody stools, abdominal pain, tenesmus, growth failure, oral ulcerations, rash (erythema nodosum or pyoderma gangrenosum), uveitis
- Laboratory Tests: Stool calprotectin, ESR, CRP, Stool culture, FOBT, CBC (anemia), low albumin
- Imaging: Endoscopy/Colonoscopy
- Management: immunosuppression/immunomodulation
PFAPA/Periodic fevers
- Signs/Symptoms: Recurrent high fevers, aphthous ulcers, pharyngitis, adenitis, asymptomatic between flares
- Laboratory Tests: no diagnostic laboratory test, can have elevated inflammatory markers (CRP and ESR) and leukocytosis during episodes
- Management: antipyretics, steroids, prophylaxis with colchicine or cimetidine, tonsillectomy
Kawasaki Disease
- Complete - Diagnostic Criteria:
- Fever 5 days plus conjunctivitis, cervical lymph node >1.5cm, mucositis, rash (not vesicular), extremity changes (edema/erythema/desquamation)
- Other nonspecific symptoms: diarrhea, vomiting, irritability, cough, arthritis
- Laboratory tests if unsure: UA (Sterile pyuria), CBC (leukocytosis, anemia, thrombocytosis), CMP (hypoalbuminemia, elevated ALT) elevated ESR or CRP
- Management: IVIG + aspirin, follow up echo
Rheumatic Fever
- 2 major or 1 major plus 2 minor manifestations:
- Major: carditis, arthritis, Sydenham chorea, erythema marginatum, subcutaneous nodules
- J: joints (polyarthritis)
- O: heart problems (valvular damage, myocarditis, pericarditis)
- N: nodules (extensor surfaces)
- E: erythema Marginatum (annular pink rash with sharp, raised edges and central clearing)
- S: Sydenham chorea
- Minor: arthralgia, fever, elevated ESR or CRP, prolonged PR interval on EKG
- Major: carditis, arthritis, Sydenham chorea, erythema marginatum, subcutaneous nodules
- Management: penicillin
Infectious
- EBV, CMV
- Signs/symptoms: tonsillitis/pharyngitis +/- exudates, posterior or diffuse cervical LAD, severe fatigue, +/- hepatosplenomegaly, +/- rash after amoxicillin
- Laboratory: Monospot test, EBV/CMV PCR, CBC- diff with atypical lymphocytes
- Adenovirus
- Laboratory: serum or urine adenovirus
- Tickborne infections – Lyme disease, ehrlichiosis, babesiosis, rickettsia
- Other Zoonotic Infections
- Brucellosis
- Cat scratch disease (bartonella) – can biopsy lymph nodes
- Leptospirosis
- Malaria
- Mycobacterial (TB)
Immunodeficiencies
- Laboratory tests: Serum IgG, IgA, IgM; Functional antibody production titers, B cell flow cytometry, genetic testing, complement testing/assays, CBC with differential
- Diagnoses based on symptoms:
- B cell defects – recurrent sinopulmonary infections (particularly with encapsulated organisms), gastroenteritis (giardia or enterovirus), failure to thrive
- Examples: XLA, CVID
- T cell defects - recurrent viral infections, failure to thrive, chronic candidiasis, chronic diarrhea, PJP, eczematoid or seborrheic rashes
- Examples: SCID, Ataxia-Telangiectasia, WAS, etc.
- Phagocyte defects – poor wound healing, delayed separation of umbilical cord, abscesses, mucosal ulcerations, infection with catalase pos organisms
- Examples: Chronic granulomatous disease, Leukocyte adhesion deficiency, Chediak-higashi, Hyperimmunoglobulin E
- Complement defects – angioedema, autoimmune diseases
- B cell defects – recurrent sinopulmonary infections (particularly with encapsulated organisms), gastroenteritis (giardia or enterovirus), failure to thrive
Hematologic/Oncologic
- Cyclic neutropenia
- Signs/symptoms: periodic fever, mucosal ulceration, malaise, and other infectious/inflammatory findings including respiratory complaints, skin/oropharynx inflammation, sinus pain, lymphadenopathy
- Laboratory: ANC < 200, genetic testing
- Management: G-CSF
- Liquid malignancies (leukemia, lymphomas)
- Solid malignancies (neuroblastoma, hepatoblastoma)
Endocrinopathies
- Hyperthyroidism
- Signs/Symptoms: tachycardia, proptosis, weight changes, changes in menses
- Labs: TSH, free T4, specific thyroid auto-antibodies
- Treatment: anti-thyroid drug, radioactive iodine, or thyroidectomy
In pediatrics, fever is most often going to be due to infection, but consider “zebras” (rheumatologic, hematologic, oncologic, immunologic) if you see concerning symptoms like weight loss (acute or chronic), bloody stool, severe lab abnormalities
Click the drop down to reveal the correct answers
Q1: 4 year old with fever for 5 days presents to the emergency room. On exam, you notice palmar erythema and swelling, right sided neck swelling, and oral mucosal changes. Parents report a few days ago, the child had red eyes. What is a complication of this disease if left untreated?
Q2: 3 year old with fever for 4 days presents to the hospital because he is not eating or drinking. Review of the child’s growth chart shows weight loss. On exam, you feel enlarged lymph nodes throughout and notice that the child is very pale with scattered petechiae. What diagnosis are you concerned for?
Answers
Q1: Coronary artery aneurysm
Q2: Leukemia. Petechiae are a sign of low platelets. Pallor is a sign of low red blood cell count. Weight loss and enlarged lymph nodes are often worrying for an oncologic process
Podcasts
- https://emergencymedicinecases.com/episode-48-pediatric-fever-without-source/
- https://www.pedscases.com/approach-recurrent-fevers
- #77: Childhood-Onset SLE – Is It Sometimes Lupus? - The Curbsiders
Pathways
- Fever In the Returned Traveler — Emergency Department | Children's Hospital of Philadelphia
- Fever Clinical Pathway — All Settings | Children's Hospital of Philadelphia
- Kawasaki Disease or Incomplete Kawasaki Disease Clinical Pathway — Emergency Department and Inpatient | Children's Hospital of Philadelphia
Other Resources
- Interpreting Rheumatology Laboratory Tests | Pediatrics In Review | American Academy of Pediatrics (Can access the full article through Biomed library)

