Thrombocytopenia
A 4-year-old female with history of asthma presents to their primary care pediatrician due to new, red dots on her shins and her elbows.
Her mother reports that the patient was otherwise in her usual state of health when she developed red, non-itchy dots on her shins and her elbows approximately two days ago. Her mother also noted that she has also had multiple nosebleeds over the past few days, which she thought might have been a result of her picking her nose. She says that the patient has been feeling a little bit more tired than usual, which she had initially attributed to a bad asthma flare a couple of weeks ago secondary to a virus. Otherwise she has not had any fevers, weight loss, decreased oral intake, abdominal pain, diarrhea, bone pain, or night sweats. There is no family history of bleeding disorders or malignancy.
Internet Scientific Publications
4-month-old with new onset petechiae on bilateral lower extremities
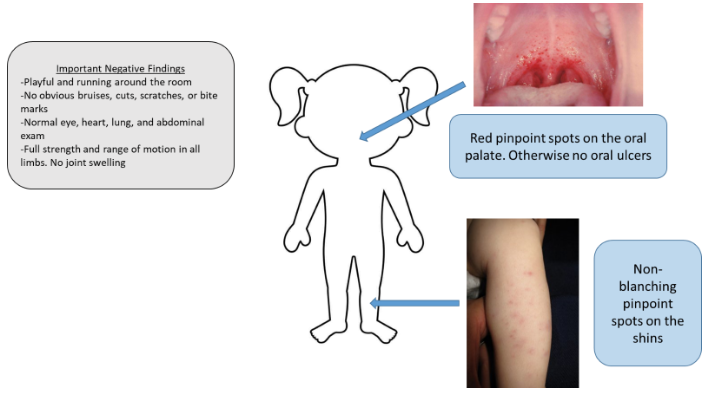
The image shows a child with red pinpoint petechiae on the oral palate and non-blanching pinpoint spots on the shins, both consistent with thrombocytopenia. A text box notes reassuring negative findings, including a normal systemic exam, no bruises or injuries, and full strength and range of motion. The overall picture highlights isolated petechiae in an otherwise well-appearing child.
Initial Evaluation
- Obtain a CBC with smear to look at hemoglobin, platelet, and white blood cell counts.
- Obtain blood smear to assess platelet levels, platelet size, and look for presence of cancer cells (blasts).
- Obtain coagulation markers in the setting of nose bleeds
Lab Results
- Labs showed white blood cells and hemoglobin within normal limits. Platelets were low at 20,000.
- Platelets were normal size on the smear, and no cancer cells were seen.
- Coagulation markers were normal
Diagnosis
Idiopathic thrombocytopenic purpura! Also known as immune thrombocytopenic purpura.
How we got there: Normal platelet levels are typically within range of 150,000-400,000. Given that this patient had significantly decreased platelets (known as thrombocytopenia) in setting of prior viral illness and is otherwise well-appearing, the most likely diagnosis is idiopathic thrombocytopenic purpura (ITP).
Management
- Consult Hematology and arrange for follow-up with Hematology (often requires watchful waiting over a course of 3 months)
- If severe, can consider:
- IVIG (prevents bleeding by slowing down the destruction of platelets)
- Steroids (prevent bleeding by decreasing the rate of platelet destruction)
- In some cases that are not as straightforward, a patient may require a bone marrow aspiration to assess platelet production
- Minimize use of NSAIDs given (reversible) anti-platelet activity
- Implement fall precautions (due to potential for intracranial bleeds secondary to low platelets in setting of trauma)
- ITP is defined by a decreased platelet count (less than 100,000) in a patient whose white cell count, red cell count, and blood smear are all normal. It is usually triggered by a viral infection or environmental factor.
- ITP can usually be treated outpatient, and most patients will recover, though some cases can become chronic.
Click the drop down to reveal the correct answers
Q1: What is the role of IVIG in idiopathic thrombocytopenic purpura?
- Slows the destruction of platelets
- Stimulates the bone marrow to produce more platelets
- Decreases risk of developing an aseptic meningitis in patient with concern for intracranial hemorrhage
- Inhibits blast formation
Q2: What are laboratory abnormalities expected in idiopathic thrombocytopenic purpura?
- Blast cells on blood smear
- Decreased hemoglobin
- Thrombocytopenia
- All of the above
Answers:
Q1: A
Q2: C

