Non-alcoholic fatty liver disease
What is fatty liver? The term “fatty liver” refers to extra fat in the liver. The liver normally has less than 5% fat. A “fatty liver” means that the liver has more than 5% fat. Typically, this fat is seen on ultrasound, CT scan or MRI; however, in some patients, it is diagnosed by a liver biopsy.
What causes fatty liver? There are many causes of “fatty liver.” Worldwide, the most common cause is from excessive alcohol consumption. In patients who do not drink excessive alcohol, “fatty liver” can be caused by viral infections, certain medications, genetic conditions, very rapid weight loss, or weight gain.
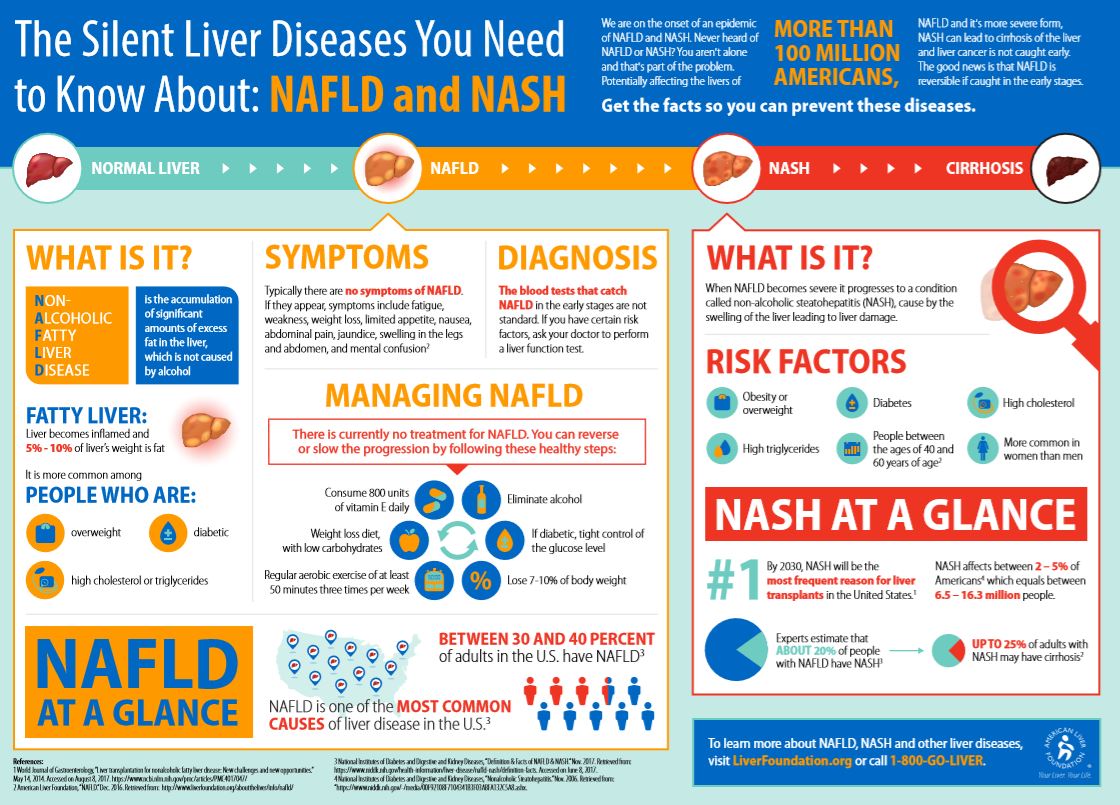
A condition called non-alcoholic fatty liver disease (NAFLD) usually refers to fatty liver that develops as a result of too much fat circulating in the bloodstream. Many of these patients are overweight or obese; have a family or personal history of diabetes, high cholesterol, or high blood pressure (metabolic syndrome); and have a reduced response to an important hormone called insulin. NAFLD affects approximately 30% of the US population.
What is NASH? NASH stands for non-alcoholic steatohepatitis. This is the combination of fatty liver with liver inflammation. Some patients with NASH can develop scarring of their liver (fibrosis). Patients with liver fibrosis can also develop cirrhosis or liver cancer.
How much alcohol is too much? The amount of alcohol that is considered excessive is different for men and women. Men should consume no more than 2 drinks a day; women should consume no more than 1 drink a day.
How do I cure fatty liver? First, we recommend you seek medical care by a provider who has experience treating patients with fatty liver diseases. In general, the cure for fatty liver depends on the cause. For example, if your fatty liver is due to alcohol, then we recommend you abstain from drinking alcohol. We have provided some resources here to support those who are dependent on alcohol.
If your fatty liver is due to obesity or metabolic syndrome, we recommend dietary changes and weight loss of 10% of your current body weight. Your provider will discuss with you specific ways to achieve this goal.
Are there research studies on fatty liver? Yes, there are several ongoing studies. If you are interested in learning more about these research opportunities at the University of Pennsylvania, please discuss this with your provider and request a referral.
Patient appointments can be made by calling 215-349-8222.
Symptoms
Usually, NAFLD is a silent disease with no signs and symptoms.
However, early NAFLD symptoms may include:
- Enlarged liver
- Fatigue
- Pain in the upper right abdomen
Possible signs and symptoms of non-alcoholic steatohepatitis (NASH) and cirrhosis (advanced scarring) include:
- Abdominal swelling (ascites)
- Enlarged blood vessels beneath the skin's surface
- Enlarged breasts in men
- Enlarged spleen
- Red palms
- Yellowing of the skin and eyes (jaundice)
When to see a doctor
Make an appointment with your doctor if you are obese, with type 2 diabetes or have metabolic syndrome and if you have persistent signs and symptoms that cause you concern.
Prevention and Treatment
To prevent the risk of developing non-alcoholic fatty liver disease:
- Choose a healthy lifestyle with a healthy plant-based diet rich in fruits, vegetables, whole grains and healthy fats.
- Exercise. Exercise most days of the week. Get an OK from your doctor first if you haven't been exercising regularly
- Maintain a healthy weight. If you are overweight or obese, reduce the number of calories you eat each day and get more exercise. If you have a healthy weight, work to maintain it by choosing a healthy diet and exercising.
To treat non-alcoholic fatty liver disease:
Currently, lifestyle changes may ameliorate steatosis (1-3). Several research trials showed that weight loss is the most effective way to reduce liver fat; losing at least 3 to 5 percent of the body weight can reduce fat in the liver (4, 5) and there is evidence that ≥10% weight loss could be associated with a reduction of liver fibrosis (6-9).
The Mediterranean diet is another option for the treatment of NAFLD. Mediterranean diet is rich in vegetables, fruits, whole grains, seeds, nuts, legumes, and fish (1). This diet is rich in monounsaturated fatty acids and polyunsaturated fatty acids as well as fibres and antioxidants and has been shown to reduce hepatic fat and improve hepatic insulin sensitivity even without weight loss (10).
Physical activity is also beneficial for reducing liver fat and may be promoted in patients who find difficult to modify their diet and follow dietary recommendation (2).
Therefore, the combination of calories restriction as well as dietary pattern associated with physical activity needs to be considered in the treatment of NAFLD.
References
- EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. Diabetologia. 2016;59(6):1121-40.
- Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology. 2012;142(7):1592-609.
- Lazo M, Solga SF, Horska A, Bonekamp S, Diehl AM, Brancati FL, et al. Effect of a 12-month intensive lifestyle intervention on hepatic steatosis in adults with type 2 diabetes. Diabetes care. 2010;33(10):2156-6
- Patel NS, Doycheva I, Peterson MR, Hooker J, Kisselva T, Schnabl B, et al. Effect of weight loss on magnetic resonance imaging estimation of liver fat and volume in patients with nonalcoholic steatohepatitis. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2015;13(3):561-8.e1.
- Sevastianova K, Kotronen A, Gastaldelli A, Perttila J, Hakkarainen A, Lundbom J, et al. Genetic variation in PNPLA3 (adiponutrin) confers sensitivity to weight loss-induced decrease in liver fat in humans. The American journal of clinical nutrition. 2011;94(1):104-11.
- Vilar-Gomez E, Martinez-Perez Y, Calzadilla-Bertot L, Torres-Gonzalez A, Gra-Oramas B, Gonzalez-Fabian L, et al. Weight Loss Through Lifestyle Modification Significantly Reduces Features of Nonalcoholic Steatohepatitis. Gastroenterology. 2015;149(2):367-78.e5; quiz e14-5.
- St George A, Bauman A, Johnston A, Farrell G, Chey T, George J. Independent effects of physical activity in patients with nonalcoholic fatty liver disease. Hepatology (Baltimore, Md). 2009;50(1):68-76.
- Bellentani S, Dalle Grave R, Suppini A, Marchesini G. Behavior therapy for nonalcoholic fatty liver disease: The need for a multidisciplinary approach. Hepatology (Baltimore, Md). 2008;47(2):746-54.
- Eslamparast T, Tandon P, Raman M. Dietary Composition Independent of Weight Loss in the Management of Non-Alcoholic Fatty Liver Disease. Nutrients. 2017;9(8).
- Ryan MC, Itsiopoulos C, Thodis T, Ward G, Trost N, Hofferberth S, et al. The Mediterranean diet improves hepatic steatosis and insulin sensitivity in individuals with non-alcoholic fatty liver disease. Journal of hepatology. 2013;59(1):138-43.
Visit the American Liver Foundation to read more about NAFLD!