Jaundice
- Where to Find in the PSOM Curriculum
- Clinical Approach
- Differential Diagnosis
- Evaluation and Management
- Pearls
- Knowledge Check
- Resources
- Pre-Clerkship
- Integrative Science
- Gastroenterology
- Bilirubin, Jaundice, Gallstones
- Disorders of the Biliary Tree
- Intro to Pediatric Liver disease
- Gastroenterology
- Integrative Science
- Clerkship
- Pediatrics Clerkship - Well baby nursery
- Post Clerkship Electives that may further knowledge - Well baby nursery, NICU, Hematology, Gastroenterology
A 3-day old male born at 37 weeks and 6 days (37w6d) presents to his primary care physician with elevated bilirubin.
He was discharged from newborn nursery yesterday, and has been breast feeding every 2-3 hours, with multiple urine and stool diapers daily. Mother feels that her milk “is starting to come in.” Birth weight 3112g, today’s weight 2895g (-7%).
Birth history: born at 37 weeks via repeat C-section. No NICU stay. Mother’s prenatal labs and course were notable for gestational hypertension. Mother’s blood type is O+, antibody negative. Bilirubin at time of discharge from newborn nursery was 6.7.
Well appearing infant, sleeping comfortably in caregiver’s arms. Normocephalic; anterior fontanelle open, soft & flat. Heart RRR, no murmur. Lungs CTAB. Abdomen soft, non-tender, non-distended, no hepatosplenomegaly. No rash or apparent bruising. +scleral icterus and jaundice across face, chest & abdomen.
Clinical Approach
History:
- Birth history: gestational age, complications, maternal prenatal labs including blood type & antibody screen for both mother & baby
- How is the infant feeding? Breastmilk or formula
- How many wet diapers? What do stools look like? Pay special attention to color of stools
- Family history of liver, gall bladder, or hematologic disorders (G6PD, thalassemia, hereditary spherocytosis, etc.)?
- Did parents or siblings require phototherapy as infants?
Physical Exam
- Overall appearance
- Look for skin coloration (can press skin to blanch, look for yellow hue) and scleral icterus.
- Examine for hepatosplenomegaly, cephalohematoma, or bruising*.
- Neurologic exam, including infant reflexes.
*Note: congenital dermal melanocytosis (CDM) can look like bruising
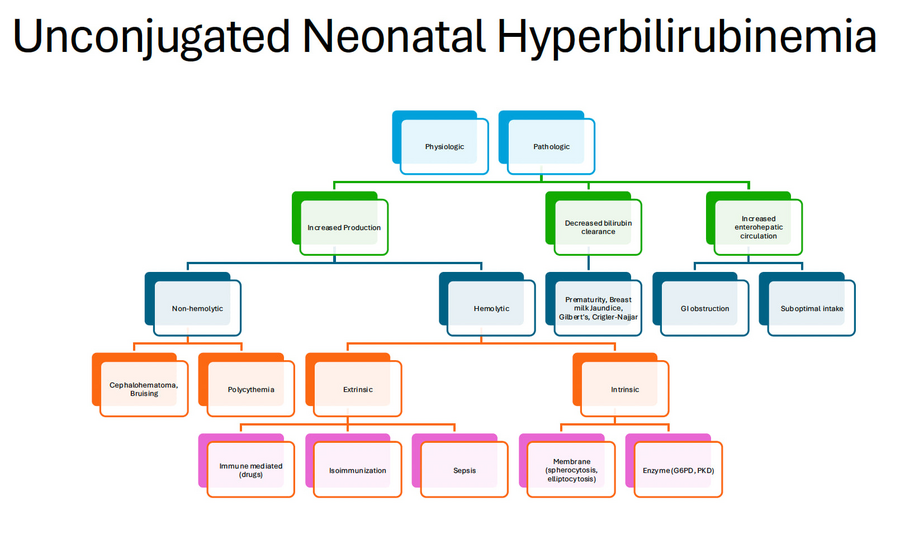
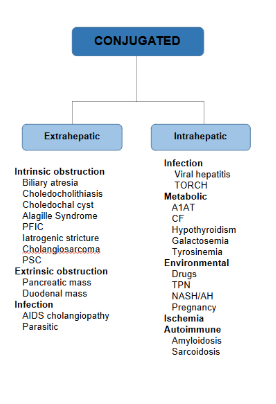
One must first determine what the infant’s bilirubin level is, and if the bilirubin is mostly unconjugated or conjugated. In most cases, hyperbilirubinemia in a newborn will be unconjugated (see below). Conjugated hyperbilirubinemia should ALWAYS trigger further work up, as the infant could have a biliary obstruction, which is an emergency – significant delays in surgical repair (if indicated) have been associated with worse outcomes.
Why do we care about bilirubin? A degree of jaundice or hyperbilirubinemia (elevated bilirubin) is physiologic (meaning that it’s a normal process for newborns), and is a result of the infant learning how to feed and for their body to learn how to breakdown & eliminate blood products. However, when the bilirubin levels gets too high, the infant is at risk of kernicterus, which is bilirubin-induced neurologic damage such as developmental delays, hearing loss, and movement disorders. Prompt initiation of phototherapy when indicated drastically reduces the risk of kernicterus.
- Measure bilirubin level (can screen with transcutaneous level but if elevated >15mg/dL, will need to obtain serum bilirubin level).
- May need to obtain CBC, reticulocyte count, infant blood type & DAT (Coombs antibody test); if requiring escalation of care, may need blood type & screen, albumin level.
- Determine risk factors for hyperbilirubinemia, including: gestational age <40 weeks, jaundice within first 24h of life, phototherapy during newborn admission, family history of parent or sibling requiring phototherapy, hemolysis, exclusive breastfeeding with suboptimal intake, among others.
- Determine neurotoxicity risk factors, including: gestational age (if <38 weeks), iso-immune hemolytic disease (such as ABO incompatibility, G6PD deficiency), clinical instability or sepsis
- Plot infant’s information on BiliTool™ to determine phototherapy level (also called phototherapy threshold)
-
- If bilirubin level is at or near phototherapy level, initiate phototherapy – often “triple phototherapy” with 2 sets of multiple lights + bili blanket.
-
- Example from BiliTool if this infant’s bilirubin at 72 hours of life (HOL) is 20.0:


- In this case, because the infant’s bilirubin level is ABOVE phototherapy threshold of 18.1, we would start phototherapy. Because mother’s blood type is O (which places baby at risk of ABO incompatibility), would obtain infant CBC, retic, blood type & DAT (Coombs antibody test). This baby is well below the exchange transfusion threshold – if numbers were closer, would need to discuss with NICU.
- Other causes of concern would be a high rate of rise (increase in bilirubin 0.2/hour or higher)
Continued Management
- Repeat bilirubin level after several hours on phototherapy
- If bilirubin level is appropriately decreasing and below the level used to initiate phototherapy, can discontinue phototherapy.
- Not every infant will need a “rebound” bilirubin level – this is a level obtained several hours AFTER phototherapy is stopped, to see if or how quickly the infant’s bilirubin rises after therapy is stopped. Only infants with risk factors (such as ABO incompatibility) may need a rebound level.
- Most of the time, neonatal hyperbilirubinemia is physiologic and responds appropriately to hydration (which helps infants clear the bilirubin in their stool) and phototherapy. Formula supplementation is not a necessity in most cases, and should always be a discussion with caregivers if caregiver's goal is to breastfeed their infant.
- We cannot determine an infant’s bilirubin level by their skin alone! You may come across charts delineating relative level of bilirubin based on the extent of jaundice – but these are not accurate, and we should instead use the measured level (either transcutaneous or total serum bilirubin).
- Other mimics of jaundice include carotenemia, which is a yellow/orange tint to the skin from excessive consumption of beta carotene. This is most often seen in older infants once they start eating pureed foods, or in toddlers.
Click the drop down to reveal the correct answers
Q1: A 3-day old infant presents to the Emergency Department for bilirubin evaluation. The infant was born at 37 weeks and is exclusively breastfeeding with at least 3 wet diapers daily. Mother’s blood type is O+. The infant’s serum bilirubin level is 20.0 (all unconjugated), which is above the phototherapy threshold of 18.1. In addition to starting phototherapy, which of the following labs would be most helpful to obtain?
- Electrolytes
- Infant blood type and DAT
- Repeat mother’s blood type
- Hepatic function panel
Answer:
Q1: (b) infant blood type & DAT, as infant is at risk of ABO incompatibility with mother’s blood type O. There is no indication to obtain electrolytes or hepatic function panel at this point.

