Vomiting
- Where to Find in the PSOM Curriculum
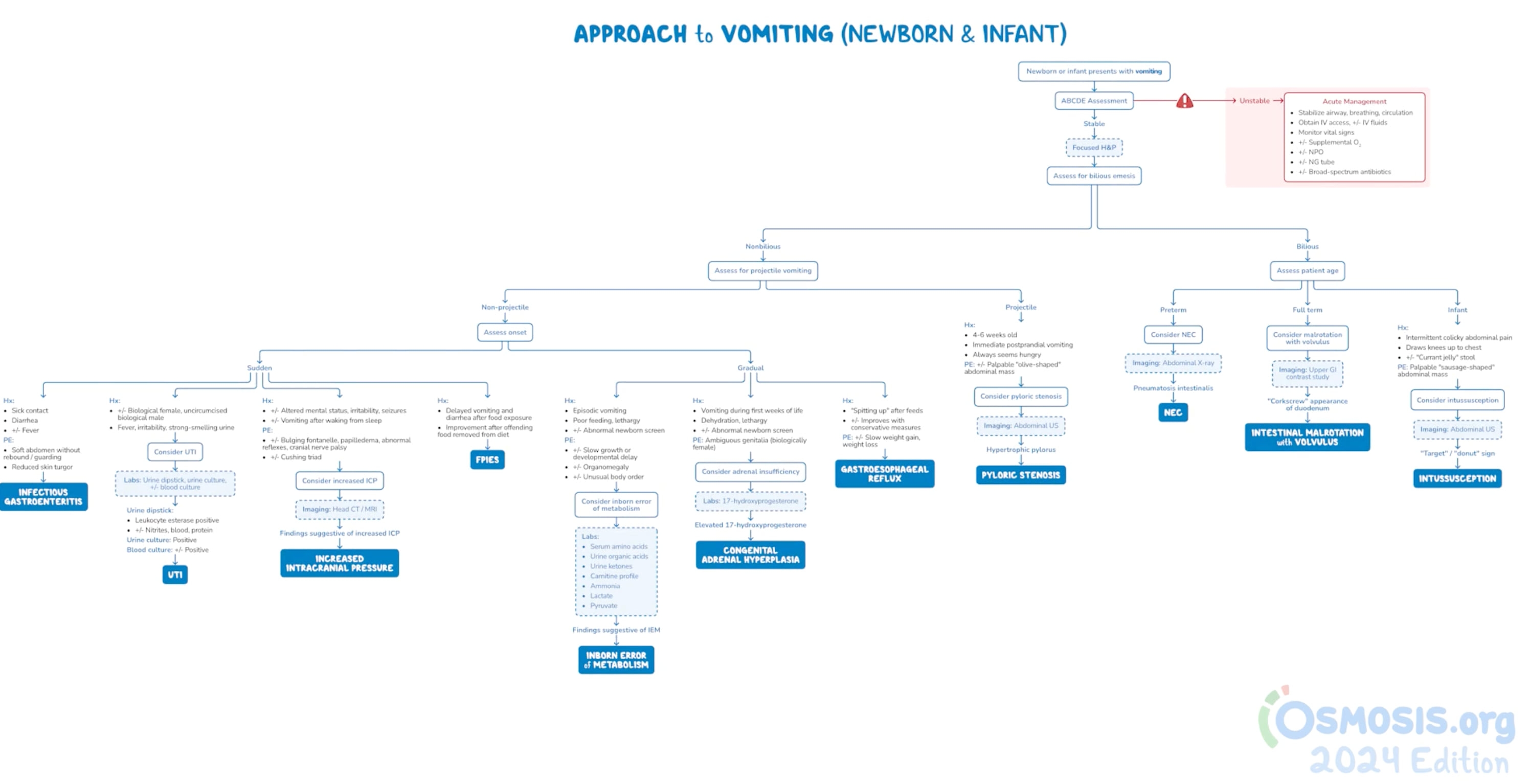
- Clinical Approach
- Differential Diagnosis
- Evaluation and Management
- Pearls
- Knowledge Check
- Resources
- Core 1 (Pre-Clerkship)
- Biomedical Science
- Biochemistry
- Metabolic lectures
- Anatomy
- The Alimentary Tract and GI Circulation
- Biochemistry
- Integrative Systems
- Gastroenterology
- Alimentary and Para-alimentarly Tract Embryology
- Gastroenterology
- Biomedical Science
- Core 2 (Clerkship)
- Pediatric Clerkship Pediatrtic Emergencies Didactic
- Core 3 (Post Clerkship) Electives that may further knowledge - Well baby nursery, NICU, GI, Primary Care
Clinical Vignette:
A 6-week old male born full-term presents with vomiting.
Parents state that since birth, he has had small spit ups after most feeds. Over the past week, his spit ups have become more forceful and larger volume, occurring after feeds. Vomit is non-bloody and non-bilious (NBNB). He takes 3oz formula every 3 hours and parents state that his pediatrician thinks he has been growing well. He has several wet and poopy diapers daily. No reported fever or looser stools.
Well appearing infant, interactive with examiner. Anterior fontanelle open, soft & flat. Abdomen soft, non-tender, non-distended, no hepatosplenomegaly, +small olive-shaped mass in upper abdomen. Normal newborn reflexes.
History
- Vomit details: when did vomiting start? How many episodes of vomiting? Is vomiting forceful or projectile (i.e. shooting across room)? What does vomit look like (bloody or bilious)? When does vomiting happen – any association with feeds?
- Feeding: what does infant take (breast milk, formula)? How much and how often? Look for signs of overfeeding or aspiration.
- Stools: how often are they stooling? What do stools look like (color, consistency)? Any abdominal distension or discomfort?
- How has infant been growing? Any weight concerns?
Physical Exam
- Overall appearance
- Ideally observe feed to evaluate suck/swallow pattern. Evaluate for suck.
- Abdominal exam – look for distension, discomfort, signs of obstruction, or mass.
- Careful neurologic exam – examine fontanelle, look for signs of elevated ICP (altered mental status, bulging fontanelle, Cushing's triad of bradycardia, hypertension, irregular respirations)
All babies will spit up – the key is determining if spit up/vomiting is physiologic or pathologic!
Physiologic spit up/vomiting: due to naturally loose esophageal sphincter in infants and gravity (i.e. laying a baby down after feeding, liquid will naturally come back up). Baby should still be gaining weight well and not in significant discomfort (i.e. “happy spitters”). Post-tussive emesis (vomiting after coughing) is also common in children.
Pathologic spit up/vomiting: when vomiting is interfering with growth or comfort, or if there are red flags on exam or history. Red flags include:
- Forceful or projectile vomiting
- repeated vomiting
- vomit that is bloody or bilious (bright green)
- concerns for dehydration (such as decreased wet diapers)
- lethargy, poor feeding
- extreme discomfort, distended abdomen
The presence of red flags should raise concern for pathologic causes of vomiting, including:
- bowel obstruction or anatomic abnormality (such as pyloric stenosis, intestinal malrotation or volvulus – obstructions are surgical emergencies!)
- necrotizing enterocolitis (NEC, especially in premature infants)
- gastrointestinal reflux disease (GERD)
- milk protein allergy or intolerance
- metabolic condition or inborn error of metabolism (IEM).
- In isolated vomiting, you must also consider elevated intracranial pressure (ICP) or UTI.
Differential diagnosis of vomiting by mechanism
|
Mechanism |
Possible Diagnosis |
Illness Script |
|
GI obstruction |
Pyloric Stenosis |
3-6 weeks of age, first born males; projectile, nonbilious, emesis, infants are hungry; Hypochloremic, hypokalemic metabolic alkalosis
|
|
Malrotation with volvulus |
Bilious emesis in less than 1 month old, ill appearing, Surgical emergency
|
|
|
Hirschsprung’s disease |
Aganglionic colon Failure to pass meconium within first 24 hours, but presentation is variable
|
|
|
GI disease |
Milk allergy |
Due to large MW proteins in cow’s milk; Blood tinged stools or emesis, heme + stools’ Elevated eosinophils |
|
GERD |
Common in infants, due to low LES tone |
|
|
Acidosis |
Inborn errors of metabolism |
Lethargy, poor weight gain, seizures, hypotonia |
|
Due to infection |
UTI, meningitis, gastroenteritis, AOM |
Fever, poor feeding, and symptoms depending on the illness |
|
Elevated ICP |
Congenital hydrocephalus |
Large head circumference, increasing in size, bulging fontanelle |
|
Renal causes |
Posterior urethral valves |
Hydronephrosis, oligohydramnios, poor urinary stream, no void in first 24 hours |
|
Post-tussive emesis |
Bronchiolitis, Pertussis |
Cough until vomits, signs of respiratory distress |
|
Psychosocial issues |
Overfeeding |
Screen for post-partum depression, feeding history |
Evaluation
- Physical exam – pay close attention to the abdomen (is it distended? Is the baby in discomfort with palpation? Can you feel any masses?). Review growth chart to determine if baby is continuing to gain weight & their trajectory. Careful neurologic exam.
- Consider basic lab work (such as electrolytes) if you are concerned about dehydration or significant vomiting. Keep an eye out for acid-base disturbance (metabolic alkalosis from vomiting stomach acid), electrolyte abnormalities (hypoK, hypoCl), and AKI. Review the baby’s statewide newborn metabolic screen!
- Consider abdominal X-ray, pyloric ultrasound, or upper GI series to evaluate for obstruction or anatomic abnormality. If there are neurologic concerns, obtain brain imaging to evaluate for elevated ICP.
Management
- If exam or imaging raises concern for surgical emergency, make the baby NPO (nothing by mouth) and consult Surgery.
- Start maintenance IVF
- Consider decompression with a sump from above or red rubber catheter from below
Clinical Vignette:
Pyloric ultrasound was obtained in this 6 week old, and showed pyloric stenosis. Baby successfully underwent surgical repair.
- It can difficult to differentiate between physiologic and pathologic vomiting, especially if there is a high level of concern from caregivers or the infant looks well! All infants will have some spit ups, which is completely normal. Most infants will outgrow reflux by 1 year of age. All gastroesophageal reflux (GER) does not equate to gastroesophageal reflux disease (GERD). Reflux precautions include positioning the baby upright for at least 20 minutes after feeding, and frequent burping. Antacids (such as famotidine) are not necessarily indicated, but can be trialed if the infant appears uncomfortable with feeds. Switching formula to a hydrolyzed version can also be trialed.
- An “olive shaped mass” in the upper abdomen, or “forceful” or “projectile” vomiting are hallmarks of pyloric stenosis. If a situation mentions this, be on the lookout for pyloric stenosis, which is hypertrophy or overgrowth of the pyloric sphincter. This most often presents in first-born males, around 6 weeks of age, and is treated surgically. There is an association with macrolide use (azithromycin, erythromycin).
Click the drop down to reveal the correct answers
Q1: You are called to evaluate a 1-day old infant in the newborn nursery. His nurse reports one episode of “grassy green” vomit. What is the next best step after evaluating the infant?
- Obtain upper GI series
- Allow the infant to feed
- Reassure parents that vomiting in newborns is normal
- Send newborn metabolic screen
Answer:
Q1: (a) obtain upper GI series, as bilious emesis in an infant is highly concerning for malrotation with volvulus. This is a surgical emergency, so reassurance, allowing the infant to feed, and sending a metabolic screen that takes several days to result, are not the most appropriate next steps.

