CARE-7 Curriculum
It is so gratifying to hear from students what they value about CARE-7. They appreciate learning useful clinical skills, having spaces to process their own emotions, and connecting with their patients on a deeper level.
– Alana Sagin, MD, FAAHPM, CARE-7 Director
Best practices in the design of the CARE-7 Palliative Care Curriculum include clinical exposure to patients with PC needs, inclusion of teachers of various specialties and disciplines, and creating safe and inclusive learning environments.
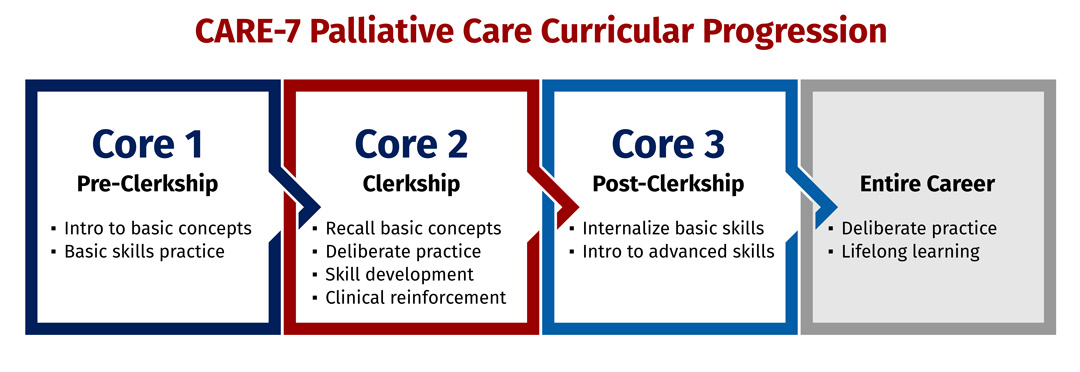
CARE-7 courses are mandatory and employ a standard stepwise approach. During Core 1 pre-clerkship, students are introduced to key concepts and skills and exposed to clinical palliative care. During Core 2 clerkship, they build on this knowledge, learning more advanced skills and concepts, which they are prompted to apply clinically. During Core 3 post-clerkship, they practice advanced skills with opportunities to pursue additional training through electives.
Students learn through both direct patient care and simulation. Simulation, which is recommended for communication skills training and in other domains, comprises both simulated patients and filmed scenarios. CARE-7 coaches and other facilitators are available for coaching and mentoring as needed.
Because of its national reputation as a leader in serious-illness communication training, CARE-7 uses the VitalTalk program. VitalTalk emphasizes strategies such as personal goal setting, group learning, safe learning environments, and the deliberate practice of communication skills to create learners who are excited and motivated to try new ways of communicating and then reflect on their own practice.
Sample Curriculum
September 1, 2023 (Subject to Change)
Introduction to Palliative Care: Part One (Year 1)
Interactive lecture describing the field of palliative care and the general outline of the CARE-7 curriculum. Importance of tracking patient/caregiver emotion and responding empathically is emphasized, and students practice using basic simulation techniques.
Introduction to Palliative Care: Part Two (Year 2)
Interactive lecture describing the field of palliative care in further depth. Introduces evidence behind the palliative care approach and discusses disease trajectories for common illnesses and how palliative care may be applied.
Palliative Medicine Experience (Year 2)
Immersion experience in which students follow a PC provider during at-home or inpatient palliative care service (e.g., at the Hospital of the University of Pennsylvania, Presbyterian Hospital, Pennsylvania Hospital, or the VA) or during home hospice visits. Immersion is followed by written reflection and Doctoring small group session for debriefing the experience.
Delivering Serious News (Clerkship Practicum)
Interactive small-group session on communication skills during Palliative Care Skills Practicum Day. Students participate in a didactic session on delivering serious news and responding to emotion, then break into small groups for skills practice using multiple filmed unfolding cases.
Pain and Symptom Management Session (Clerkship Practicum)
Interactive small-group session on pain and symptom management during Palliative Care Skills Practicum Day. Students watch a recorded didactic session on pain management for serious illness and take a pre/post quiz. They participate in a subsequent session with further didactic content in pain and symptom management and a view a filmed case. Students problem solve answers in small groups as the filmed case unfolds.
Coping With Serious Illness and End of Life (Internal Medicine Clerkship)
Narrative medicine small group session focused on processing students' emotions around patients' deaths or experiences with illness. Students read and discuss a poem and are prompted to write about their experiences caring for patients with serious illness on the wards. Students share with the group and have a facilitated discussion about coping strategies.
Palliative Care Assessment (Surgery Clerkship)
Students watch a brief video in which Chief of Trauma Surgery Niels Martin, MD, introduces the importance of primary palliative care for all surgical patients and models a palliative care assessment. He asks patients about their various domains of suffering, including pain and symptoms, their psychosocial and spiritual states and needs, and their illness experience and understanding. Clerkship students then choose a patient with serious illness, conduct their own palliative care assessment, write a brief note in the chart, and a prepare a reflection on the experience. They may bring any actionable issues they uncover to the rest of the care team.
Goals of Care Part One: Drills (Measey Track, Year 4)
Two-hour session includes a didactic teaching that introduces the REMAP framework for discussing goal of care followed by small group sessions where students use drills-practice techniques with evolving cases.
Goals of Care Part Two: Skills Practice (Measey Track, Year 4)
Session provides a chance to practice the skills learned in Goals of Care Part One through a high-fidelity simulation VitalTalk experience. Session typically includes a brief didactic refresher recalling the REMAP framework for discussing goals of care, then students break into small groups for skills practice using simulated patients in a virtual setting.
Nuts and Bolts of End-of-Life Care (Year 4)
Session on identifying the dying process, managing symptoms at the end of life, providing anticipatory guidance, and responding to common family concerns.
Palliative Care Clinical Elective
Two-week clinical elective on an inpatient palliative care consult service.
Palliative Care Concentration
Students wishing to further their knowledge may pursue a concentration in palliative care. Applications must be submitted by the end of the Core 2 clerkships.
Palliative Care Specialty Interest Group
The Specialty Interest Group organizes palliative-care-related activities and hosts multiple events per year. Events have included a "Palliative Care Career Pathways" faculty panel discussion and sessions on grief and bereavement. Projects have included the Last Writer's Program, which paired student volunteers with hospice patients to help them write their memoirs.

