Dehydration
Key Conditions
- Core 1 (Pre-Clerkship)
- Microbiology and Infectious Diseases
- GI bacteria
- Renal
- Water Balance and Control of Osmolality
- Disorders of Water Balance 1: Hyponatremia and Hypotonicity
- Disorders of Water Balance 2: Hypernatremia and Hypertonicity
- Small Groups: Sodium Balance and Volume Status Case
- Acute kidney injury pathophysiology
- Microbiology and Infectious Diseases
- Core 2 (Clerkships)
- Pediatric Clerkship Didactics on the Acutely Ill Child
- Pediatric Emergency Medicine didactics on Pediatric Trauma
- Core 3 (Post-Clerkship)Electives that may further knowledge
- Peds SubI, PEM SubI, Pediatric Nephrology, PICU, NICU
The PCP office gets a call from a parent concerned about their 9 month old daughter. Their 4 year old son seems to have “caught a GI bug” at daycare and has been having some vomiting and now diarrhea, but otherwise is appearing okay. Their 9 month old started throwing up last night and is continuing this morning. She is tired appearing and has not had a wet diaper since yesterday afternoon. She is not interested in food or her bottle – she had a few sips this morning and then threw up again.
What other questions do you want to ask this family? What should they do next?
Assessing intake:
- Feeding how often and how many ounces per feed?
- If breastfeeding, can’t determine exact volumes, but generally: how long is the baby spending breastfeeding per side? Different from typical?
- Formula mixing: often helps to start by asking open-ended (“how are you mixing the formula?”)
-
- What we need to know:
-
-
- What is the ratio of ounces of water to scoops of formula?
-
-
-
-
- This will depend on the formula and if fortified to higher calories! Standard is 20 kcal/oz. Ask which formula is being used
-
-
-
-
-
- For MOST formulas, we want 2 oz water for each scoop of (dry) formula
-
-
-
-
- What is being added into the bottle FIRST? Water or powder?
-
-
-
-
- Should be WATER! Should be adding powder TO water. This way we know the exact volume of fluid.
-
-
- Assessing output: vomiting
-
- How often is patient having vomiting or diarrhea?
-
- If vomiting, any blood or green color to it? Think of surgical abdomen emergencies in the differential, if bilious.
-
- How often is this happening? Timing related to feeds?
- Assessing output: urine and stool
-
- How many wet diapers up to the current point in the day? How many typically?
-
- For toilet trained children, appearance of urine? When was the last time they went to the bathroom/how many times today?
-
- If having diarrhea, how many times today? Appearance of stool, any blood or mucus? Sometimes harder to recognize constipation – ask about last bowel movement, typical pattern of stooling.
- Associated symptoms:
-
- Any sick contacts? In school/daycare?
-
- Always ask about presence and duration of fever
-
- Longer duration of fever (5 days or more) should always trigger more questions (i.e. assess for major criteria of Kawasaki disease)
-
- Other possible pertinent positives/negatives: rash, abdominal pain, cough/cold symptoms, dysuria, headache or other neurologic changes (don’t want to miss evidence of increased intracranial pressure)
- Always check the growth curve! Is the child falling off weight or height curve?
|
|
Description |
Where to look |
|
General Appearance |
How does the patient generally look? This is very important. Do they appear tired? Cranky but consolable by their parent? Playing with toys? Or – and this should raise concern – listless, lethargic? |
Start looking from the doorway before you approach!
It can be helpful to ask the parent how their general behavior has been that day |
|
Mucous membranes |
“Moist” vs. “tacky” - but what does this mean? Are their lips dry/cracked or sticky or wet? How about their tongue/gums? Looking at their conjunctiva, are there tears when crying? Do the whites of the eyes seem moist? Do the eyes appear sunken? |
Eyes, lips, inside the mouth |
|
Capillary refill and pulses |
Capillary refill should be < 2 seconds. Squeeze and let go of the nailbed and observe how long it takes for color to be restored after blanching.
Distal pulses: assess strength - dorsalis pedis on the dorsum of the foot, radial in wrist, brachial in arm for infants |
Fingers and toes Distal pulses in extremities |
|
Anterior fontanelle in infants |
Run fingers over anterior fontanelle – does it feel flat which is normal, or sunken? |
Top of head |
Based on these exam findings, can estimate degree of dehydration:
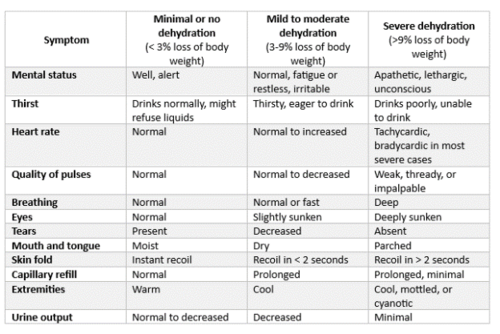
Source: https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5216a1.htm#tab1
The table outlines how dehydration severity progresses from minimal to mild–moderate to severe, with changes in mental status, thirst, heart rate, pulses, breathing, exam features, extremities, and urine output. Mild dehydration shows subtle findings such as increased thirst, slightly sunken eyes, dry mouth, and decreased tears, while severe dehydration presents with lethargy, poor drinking, weak pulses, deep breathing, sunken eyes, delayed capillary refill, cool mottled extremities, and minimal urine output. The layout offers a quick comparison to help determine severity based on physical exam.
Hypernatremia and Hyponatremia
- Hydration and fluid status does not exist in isolation: when your fluid status is abnormal, you run the risk of disrupting the electrolyte balance in your body too. One of the most significant electrolytes we worry about is sodium. In fact, serum sodium abnormalities are a reflection of water balance!
- 2 important terms
-
- Osmolality = concentration of solute (particles) dissolved in a solution
-
-
- Serum Osmolality in the human body = (1.8 * Na) + (Glucose /18) + (BUN / 2.8)
-
-
-
- Big take away = sodium has a big effect on serum osmolality!
-
-
- Tonicity = the affect a solution has on a cell based on movement of water
-
-
- Hypertonic solution: causes water to move out of a cell --> cell shrinks
-
-
-
- Hypotonic solution: causes water to move into a cell --> cell swells
-
- Sodium can be tricky – having low salt can be from being volume UP or volume DOWN... HUH? Let’s look into this more.
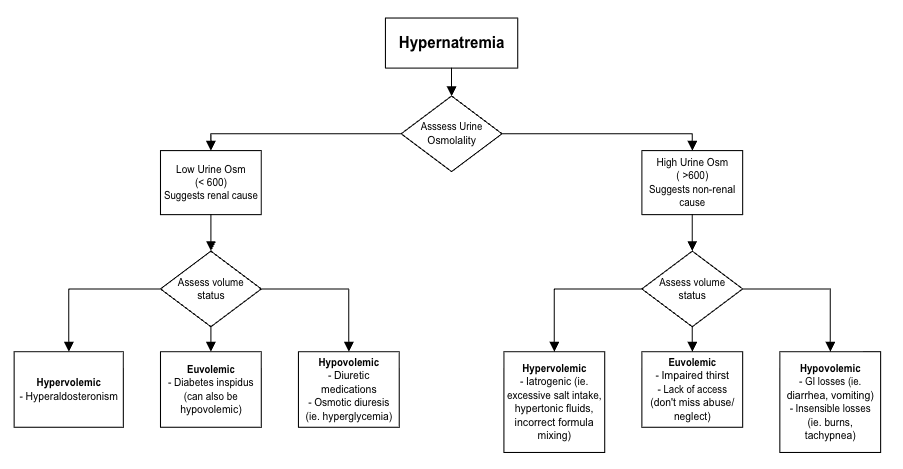
Hypernatremia
- Generally Na > 150 mEq/L in extracellular fluid (ECF)
- Three buckets
- Not enough water in
- Too much water out
- Increases in salt "in" (rare)
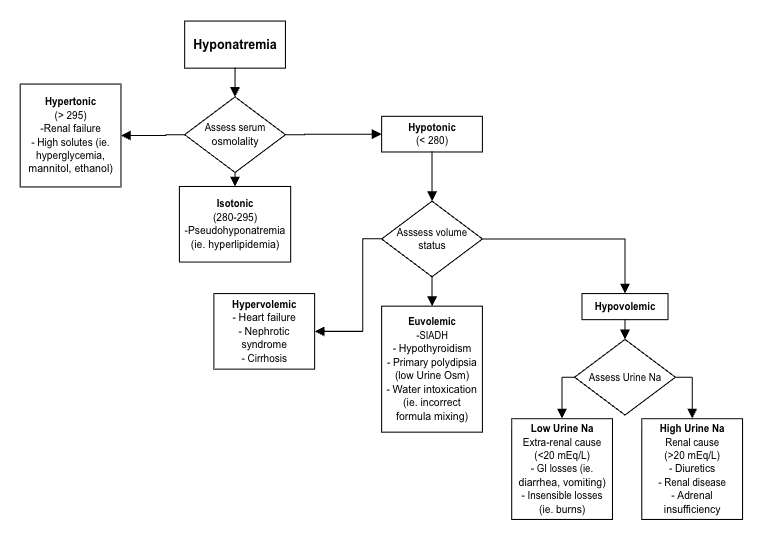
Hyponatremia
- Generally Na < 130 mEq/L in extracellular fluid (ECF)
- Three buckets
- Too much water in
- Not enough water out
- Dysregulated ADH
Two specific disease processes:
SIADH vs DI
Let’s focus on two specific disease processes that can result in water and salt dysfunction
First remember back to physiology:
- Body experiences dehydration (low blood volume or high blood osmolality) -->
- Hypothalamus senses an issue in water balance -->
- Tells Posterior Pituitary Gland to make Anti-Diuretic Hormone (ADH) and release into blood stream -->
- ADH acts on Kidney (at the distal convoluted tubule & collecting duct) -->
- Add Aquaporin or water channels into cell membrane -->
- Water reabsorbed from urine --> blood stream
- Net result: serum contains more water, urine gets more concentrated
|
|
SIADH: Syndrome of Inappropriate ADH |
DI: Diabetes Insipidus
Newer terminology: Arginine Vasopressin Deficiency (AVP-D) or Resistance (AVP-R) |
|
Pathophysiology |
Body makes too much anti-diuretic hormone (ADH) --> body holds onto too much water --> diluting effect |
Body does not make enough anti-diuretic hormone (ADH) or respond appropriately to ADH --> body gets rid of too much water --> dehydrating effect |
|
Presents as |
Excessive thirst! Hypotonic serum osmolality Hyponatremia Decreased urine output Concentrated Urine Headache, in severe cases confusion --> coma |
Excessive thirst! But consider that many pediatric patients (including infants, patients receiving tube feeds) do not fully control their own liquid intake to act when thirsty. Hypernatremia Increased urine output Dilute Urine |
|
More Specifics |
Risk factors can include: severe stress or pain, pulmonary or CNS disease, post-operative status, medications (including SSRIs, AEDs like oxcarbazepine, opiates). Think of these risk factors in many of your hospitalized patients! |
-Central DI: issue in the brain (hypothalamus or pituitary gland), where pituitary gland does not make enough ADH
-Nephrogenic DI: issue in the kidneys (intrinsic issue with kidney receptor or acquired from a medication like lithium) where kidneys don’t respond appropriately to ADH |
|
Treatment |
Address underlying cause (ie. treat pain or pneumonia) Restrict Fluid Increase salt intake Rarely use of vasopressin receptor antagonist medications that can block ADH (ex: Tolvaptan) |
Nephrogenic DI: Fluid management. Depending on cause can consider medications (ex. Thiazide diuretic) and low salt, low protein diet.
Central DI: Give Synthetic ADH (ex: desmopressin/DDAVP, can give intranasal vs oral vs subcutaneous injection) |
Hypernatremia
Identifying Cause
- Check urine osmolality to differentiate renal and non-renal causes
- Assess volume status
- Can also check urine sodium
Management
- Correct Sodium slowly! Calculate and gradually replace free water deficit
- If you correct hypernatremia too fast, you can cause cerebral edema
- "High to Low your brains will blow"
Hyponatremia
Identifying Cause
- Check serum osmolality (Osm)
- Assess volume status
- Can check urine osmolality, urine sodium
Management
- If you see an acute change in sodium (> 10 mEq drop) or symptomatic hyponatremia (ex: coma or seizure): Act now! Give hypertonic saline (IV 3% NaCl)
- If asymptomatic and chronic, first diagnose what is going on, and then correct sodium slowly!
- If you correct hyponatremia too fast, you can cause central pontine myelinolysis
- “Low to High your pons will die”
Dehydration
- Oral fluids – if able to tolerate some oral intake, either with or without receiving an anti-emetic medication like ondansetron, can trial oral rehydration therapy giving small amounts of fluid every 5 minutes.
- IV Fluids
- Fluid boluses to address fluid deficit/losses are usually 20 mL/kg (maximum 1L). Consider 10 mL/kg if fluid sensitive, such as a patient with cardiac history.
- Maintenance fluids are continuous fluids to meet ongoing physiologic needs, including urine losses and insensible losses like sweat.
- The 4-2-1 rule for maintenance rate:
- Hourly fluid rate = 4 x (first 10 kg of patient weight) + 2 x (next 10kg of patient weight) + 1 x (remainder of patient weight)
- For example, hourly rate for a 21kg child = (4 x 10) + (2 x 10) + (1x1) = 61 mL/hr
- The Holliday-Seger rule for maintenance rate:
- Total daily fluid = 100 x (first 10kg of patient weight) + 50 x (next 10kg of patient weight) + 20 x (remainder of patient weight)
- For example, for a 21kg child = (100 x 10) + (50 x 10) + (20 x 1) = 1520 cc over 24 hours = 63 mL/hr
- We usually use the 4-2-1 rule much more often!
- Fluid rates are automatically calculated in Epic
- Types of IV fluids
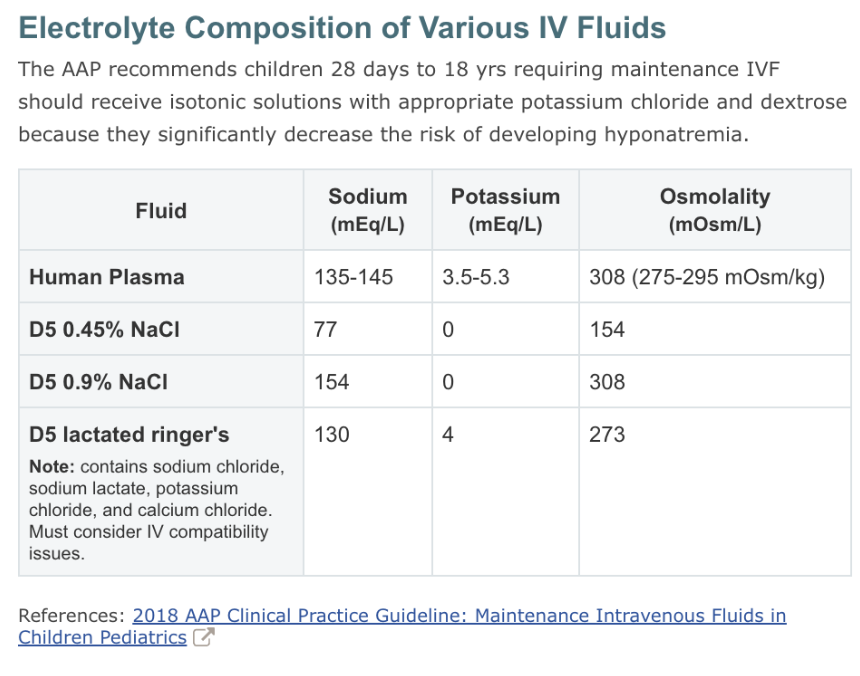
- You will commonly see/hear “D5 normal” (Dextrose 5% with 0.9% normal saline”
- Half normal = 0.45% NS
- Quarter normal = 0.225% NS (for new/tiny babies)
- KCl can be added to fluids (“D5 normal with K”). Consider 20 mEq/L KCl if weight > 10kg, 10 mEq/L if < 10kg
- You may also see D5LR: lactated ringers. This can be appealing if a patient has metabolic acidosis (ex. from GI losses) as LR contains some lactate, unlike normal saline.
- Not to memorize! Just take note of which fluid types are isotonic to human plasma and which are not
- Assessing specific intake and output in history questions is key for patients presenting with dehydration. Include specific physical exam maneuvers to assess hydration status.
- As with most interventions in pediatrics, volumes of IV fluid replacement are weight-based, both for bolus and maintenance fluids. Pediatric patients typically receive isotonic fluids.
- Abnormal sodium levels are usually related to water balance. When investigating etiology, it is often helpful to assess volume status and measurements of serum and urine osmolality.
Click the drop down to reveal the correct answers
Q1: What is the maintenance rate for IV fluids for a 14kg patient?
- 48 mL/hr
- 14 mL/hr
- 56 mL/hr
- 28 mL/hr
Q2: Which of the following would be an appropriate bolus volume for a 42kg patient without a significant cardiac history?
- 1000 mL
- 840 mL
- 42 mL
- 84 mL
Q3: Which of the following is NOT considered an isotonic fluid?
- D5NS
- NS
- D5 ¼ NS
- Lactated Ringer’s
Q4: Which of the following conditions is NOT usually associated with hyponatremia?
- SIADH
- Diabetes insipidus
- Adrenal insufficiency
- Nephrotic syndrome
Q5: Which of the following is LESS important to assess regarding intake in a formula-fed 2-month-old infant?
- how formula is being mixed
- how often infant is feeding
- how many ounces taken per bottle
- how often infant is burped
Q6: Which of the following would be an appropriate bolus volume for a 42kg patient without a significant cardiac history?
- 1000 mL
- 840 mL
- 42 mL
- 84 mL
Answers
Q1. A
Q2. B
Q3. C
Q4. B
Q5. D
Q6. B
Articles:
Videos:
Podcasts:
-
- Also comes with a 1-page summary!
Pathways:

