Clinical Experiences
The residency curriculum has been carefully designed to provide residents with a well-balanced training program emphasizing mentored individual development in the context of a wide-ranging and richly varied educational and training experience.
The core of the training program includes experience in inpatient, consultation/liaison, and ambulatory psychiatry at one of the nation's finest health systems, as well as extensive experience in outpatient psychotherapy, psychopharmacology, and combination treatment. Specialized training in psychodynamic, cognitive, behavioral, group, marital, and family therapies is a critical part of the educational mission. Residents receive exceptional instruction in emergency, addictions, community, and forensic psychiatry as well as neuromodulation and innovative models of integrated and virtual care. A substantial elective curriculum allows residents to develop their interests and take advantage of new opportunities. See below for more detailed information for each year.
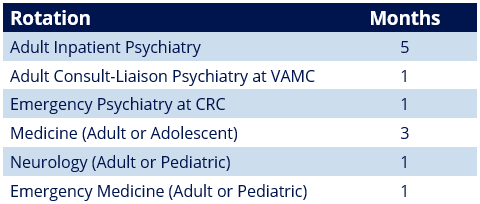
The first year of training is divided into four 3-month blocks alternating between psychiatry and off-service rotations.
Interns rotate through multiple clinical sites, including Hospital of the University of Pennsylvania (HUP), Pennsylvania Hospital (PAH), Veterans Affairs Medical Center (VAMC), Presbyterian Hospital (PPMC), and Children's Hospital of Philadelphia (CHOP).
Dedicated emergency psychiatry training is provided at HUP and the Crisis Response Center (CRC) at PAH.
Call: PGY1s are assigned to junior calls paired with a senior resident in order to gain experience before unsupervised call in the PGY2 year. Call shifts are at HUP and the CRC covering the emergency room, consults, and the inpatient units.
Vacation: 3 weeks + flex days
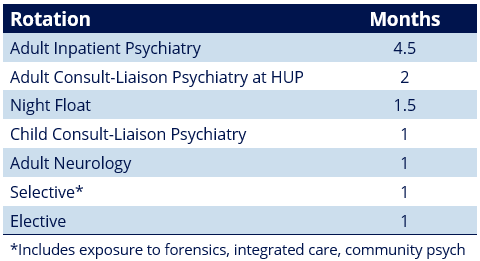
The second year builds on the strong foundation of intern year with additional inpatient psychiatry as well as selectives and resident-designed electives that allow the resident to individualize their clinical experience.
Residents begin their first outpatient psychotherapy case in January of this year, though they may begin earlier in second year if they choose.
Call: A night float rotation eliminates the need for weeknight call and improves residents' education and quality of life. In addition to night float, PGY2s serve as the senior resident paired with PGY1s for weekend shifts at the CRC, covering the emergency room, consults, and floor patients. PGY2s also do weekend solo call shifts at the VAMC.
Vacation: 4 weeks + flex days
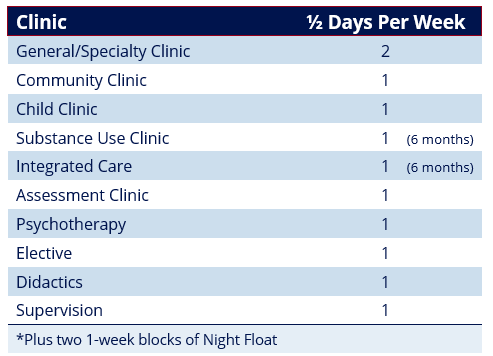
The emphasis of the third year is on ambulatory psychiatry in a variety of settings. Residents serve as providers in General Ambulatory Practice (GAP) clinics, focusing primarily on psychopharmacology. GAP clinics include general or specialty patient populations, including dual diagnosis, treatment-resistant depression, bipolar disorder, trauma, geriatric, women’s health, med-psych, anxiety, ADHD, and psychosis.
Residents provide psychotherapy through the Residents' Psychotherapy Practice (RPP). The RPP allows residents to see patients for weekly psychotherapy under the supervision of Penn's extensive clinical faculty who have a depth of expertise in a wide variety of psychotherapy modalities, including short- and long-term psychotherapies, group, couples, and family therapy.
Residents participate in an observed assessment clinic that allows residents to practice interview skills and receive feedback from peers and faculty. This clinic also provides opportunity to have in-depth group discussions on case formulation from various perspectives.
Internal moonlighting starting in PGY3 year allows senior residents to supplement their income, expand their teaching role, and maintain active engagement with the emergency and consult service at HUP and the CRC.
Call: Overall, the number of call shifts decreases significantly from PGY2 to PGY3 year, with only 6-8 weekend call shifts in the entire year. PGY3s only rotate on 2 weeks of night float. They serve as the senior resident paired with PGY1s for weekend shifts at HUP and the CRC, covering the emergency room, consults, and floor patients.
Vacation: 4 weeks + flex days
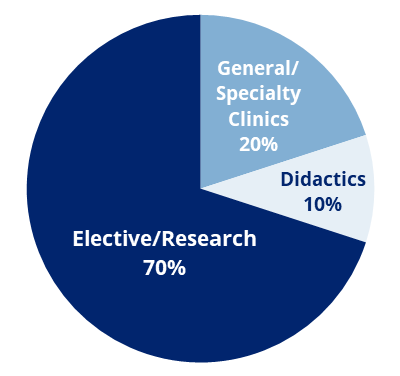
In the fourth year, each resident — under the guidance of the Program Directors and relevant faculty — develops a unique educational program that includes continued GAP and RPP clinical work, as well as intensive senior electives in areas relevant to his or her career direction. The resources of the entire department, and indeed the university, are available in the areas of clinical care, research and administration.
Residents have two days per week available for elective experiences. A Senior Teaching Requirement, focusing on the development of educational skills, a Junior Attendingship, and an Academic Project round out the year.
The Neuromodulation Rotation provides training in, and satisfies the accreditation criteria for, the provision of ECT after residency and involves experiences in Transcranial Magnetic Stimulation (TMS).
Internal moonlighting opportunities remain available to allow PGY4 residents to supplement their income, expand their teaching role, and maintain active engagement with the emergency and consult service at HUP and the CRC.
Call: PGY4 have no assigned call shifts.
Vacation: 4 weeks + flex days
Back to Top
