What is diabetic kidney disease?
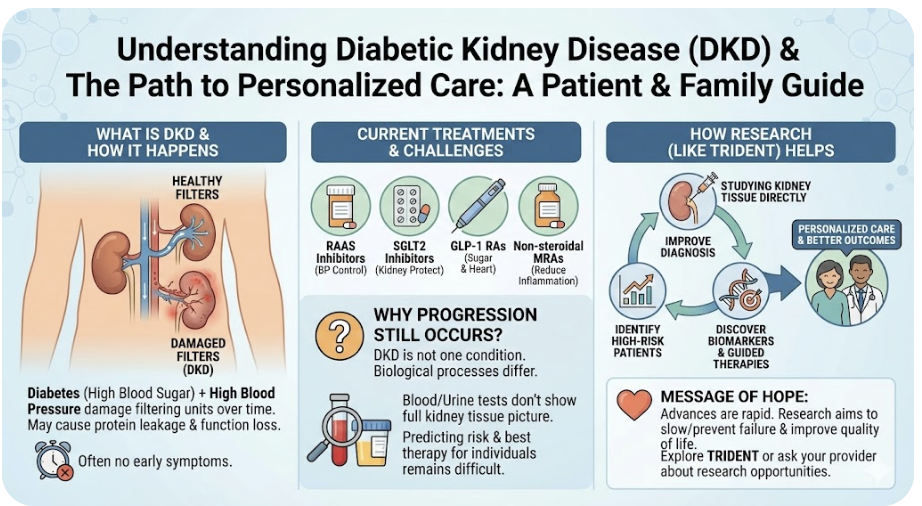
Diabetic kidney disease (DKD), sometimes called diabetic nephropathy, is a condition in which diabetes damages the kidneys over time. The kidneys act as the body’s natural filters, removing waste and excess fluid from the blood. When these filters are injured, kidney function can gradually decline.
Not everyone with diabetes develops kidney disease, and among those who do, the course of disease can vary widely. Some people maintain stable kidney function for many years, while others experience more rapid progression. Understanding why this happens is a major focus of ongoing research.
How diabetes affects the kidneys
High blood sugar, high blood pressure, and chronic inflammation can damage the small blood vessels and filtering units within the kidneys. Over time, this damage can lead to:
-
Leakage of protein into the urine
-
Gradual loss of kidney function
-
Increased risk of kidney failure and cardiovascular disease
Because early kidney damage often causes no symptoms, diabetic kidney disease may go unnoticed until it is more advanced.
Current treatments for diabetic kidney disease
Over the past decade, major advances have been made in the treatment of diabetic kidney disease. Several classes of medications are now used to slow kidney damage and reduce complications:
-
RAAS inhibitors (such as ACE inhibitors and ARBs) help control blood pressure and reduce stress on the kidneys.
-
SGLT2 inhibitors are diabetes medications that also protect the kidneys and heart by reducing kidney workload and inflammation.
-
GLP-1 receptor agonists improve blood sugar control and provide additional cardiovascular and kidney benefits.
-
Non-steroidal mineralocorticoid receptor antagonists (MRAs) help reduce kidney inflammation and scarring in selected patients.
These therapies have significantly improved outcomes, but they do not work equally well for everyone.
Why kidney disease can still progress
Even with modern treatments, some people continue to lose kidney function. This is because diabetic kidney disease is not a single condition. It reflects multiple biological processes that can differ from person to person.
Most treatment decisions today rely on blood and urine tests. While helpful, these tests do not fully capture what is happening inside the kidney tissue itself. As a result, it can be difficult to predict who is at highest risk for progression or which therapy is most likely to be effective for an individual patient.
How research studies like TRIDENT help
Research studies such as TRIDENT aim to better understand diabetic kidney disease by examining kidney tissue alongside blood and urine samples and following patients over time. By linking kidney biology to clinical outcomes, researchers seek to:
-
Improve early and accurate diagnosis
-
Identify patients at higher risk of disease progression
-
Discover new biomarkers to guide treatment decisions
-
Support the development of more personalized therapies
A message for patients and families
Living with diabetic kidney disease can be challenging, but treatment options and scientific understanding are advancing rapidly. Ongoing research is helping clinicians move toward more precise, individualized care, with the goal of slowing or preventing kidney failure and improving quality of life.
If you are interested in learning more about research opportunities or participating in a study, please explore the TRIDENT study pages or speak with your healthcare provider.
© The Trustees of the University of Pennsylvania | Site best viewed in a supported browser. | Report Accessibility Issues and Get Help | Privacy Policy | Site Design: PMACS Web Team.
