SPCC Frequently Asked Questions (FAQ)
The SPCC is a Penn Medicine Center staffed by trained, licensed mental health clinicians specializing in suicide prevention care. Our clinicians are available to treat adult patients presenting to Penn Emergency Departments (EDs) or Crisis Response Centers (CRCs) who are deemed at-risk for suicide and are expected to be discharged. Our clinicians meet with patients via telehealth while patients are in the ED to deliver the Stanley-Brown Safety Planning Intervention (SPI). Then, they'll continue following up with patients via telehealth for the next four weeks, coaching patients on using and revising their safety plan and helping patients connect with outpatient care, if needed.
The Safety Planning Intervention with post-discharge telephone follow-up (SPI+) is an intervention in which clinicians collaboratively develop a personalized safety plan with the patient, following best practices, and conduct up to four follow-up calls to check-in with patients, revise safety plans, and help patients connect to outpatient care if they do not already have such care established. SPI+ has been shown in clinical trials to reduce suicide risk and increase engagement in outpatient services. In a study of 9 Veterans Affairs EDs, SPI+ decreased suicidal behavior by 45% and doubled the odds of patients attending at least one outpatient visit. In addition, SPI+ increased ED staff comfort with discharging patients with suicide risk. (click here to view study). For more information about SPI+, please visit https://suicidesafetyplan.com/.
The Safety Planning Intervention (SPI) takes approximately 45-60 minutes to complete with an adult patient who does not require caregiver assistance. In instances where caregiver assistance is needed, the SPI takes approximately 90 minutes. The post-discharge telephone follow-up sessions take approximately 20-30 minutes to complete.
Patients who present to the ED with suicidal behavior and/or suicidal ideation are at increased risk for suicide, especially during the month following discharge. Approximately half of such patients do not engage in outpatient care. Research shows SPI+ can help decrease suicidal behavior and increase connections to outpatient care, but ED clinicians may struggle to provide this evidence-based treatment due to limited time and/or training in suicide prevention. We created the SPCC as a resource for EDs and staffed it with a dedicated team of mental health clinicians specializing in SPI+ so that patients exhibiting suicide risk can receive this gold standard care within the context of the ED.
ED clinicians in our partner locations can refer any patients who meet the following criteria:
- 18+ years old
- At risk for suicide, either based on the patient’s report or your clinical assessment
- Not expected to be admitted or transferred for inpatient care
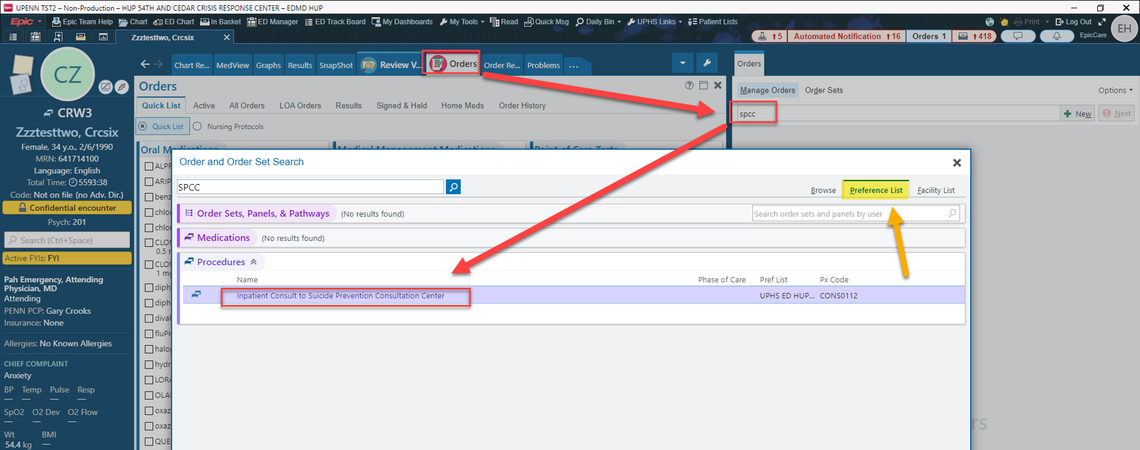
You can refer patients to the SPCC in a few easy steps:
1. Place a consult using the Inpatient Consult to Suicide Prevention Consultation Center order
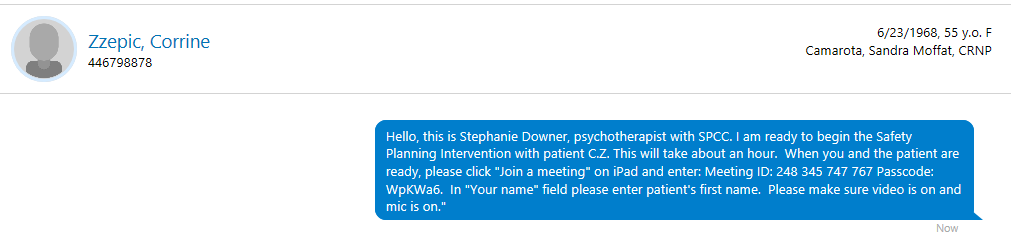
2. Our clinicians will send a Microsoft Teams Meeting ID and password to you via Epic Secure Chat
3. Retrieve one of our designated iPads (already located in the ED)

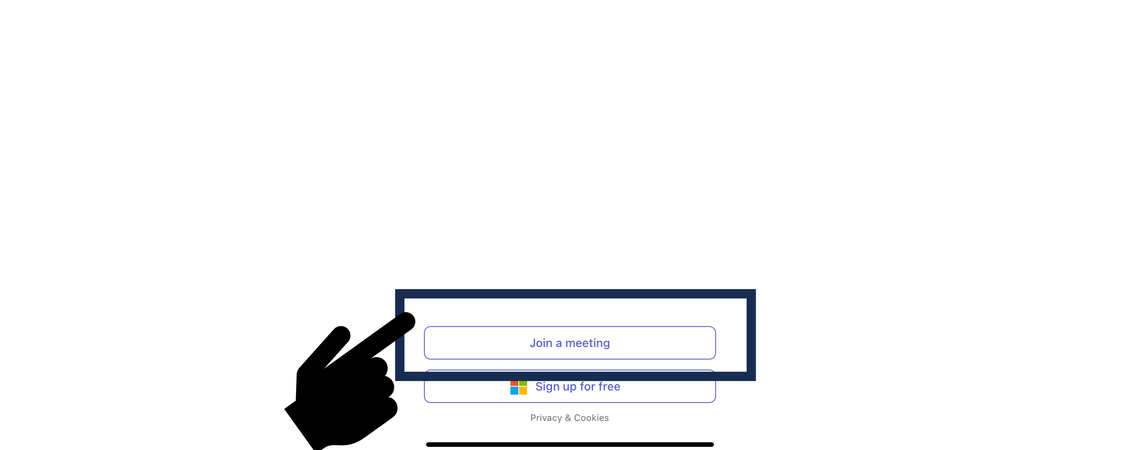
4. Open the iPad, navigate to the bottom of the Microsoft Teams page, and click “Join a Meeting”
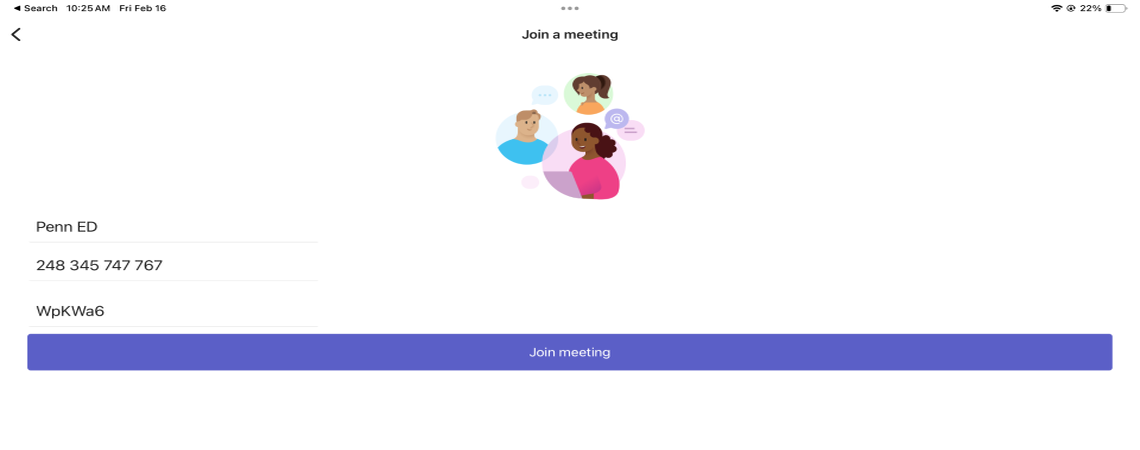
5. Login to the meeting using the meeting ID and password. Ensure the microphone and camera are both on.
6. The SPCC clinician will begin the intervention, which may take up to an hour.
7. When the SPCC clinician concludes the session with the patient, they will message you via Epic Secure Chat to update you. They will communicate any relevant clinical concerns to you.
The SPCC’s is currently accepting consult orders from 7am-10pm, Monday-Friday. We expect to increase coverage to weekends in the near future. Please check the consult order for the latest operating hours.
If you have further questions, please contact the SPCC Manager of Psychotherapy, Stephanie Downer, MA, LPC, CEAP at stephanie.downer@pennmedicine.upenn.edu or via Epic Secure Chat.
The SPCC is currently only available to participating emergency departments or crisis response centers within the Penn Medicine health system.
We are currently operating at:
- Hospital of the University of Pennsylvania at Cedar Crisis Response Center
- Penn Presbyterian Medical Center ED
- Pennsylvania Hospital ED
- Pennsylvania Hospital Crisis Response Center (CRC)
- Chester County Hospital ED
- Hospital of the University of Pennsylvania ED
- Lancaster General Hospital ED
- Princeton Medical Center ED
Our services are currently only available to patients in our partner EDs who are expected to be discharged, though this may change in the future.
Yes, patients can be referred to the SPCC multiple times. We will complete the same intervention, building on their previous safety plan, and follow up with them for up to four weeks.
Back to Top
