Murmurs
Key Conditions
- Core 1 (Pre-Clerkship)
- Anatomy and Imaging: Heart
- Cardiology: Cardiac Anatomy, Cardiac Physical Exam, Congentital Heart Disease 1, 2,
- Core 2 (Clerkship)
- Pediatric Clerkship Didactics on the Acutely Ill Child and Respiratory Pathology
- Core 3 (Post-Clerkship)
- Electives that may further knowledge: Pediatric Cardiology, Cardiology, CICU
A 6 week old presents for a well child visit. On physical exam a murmur is heard.
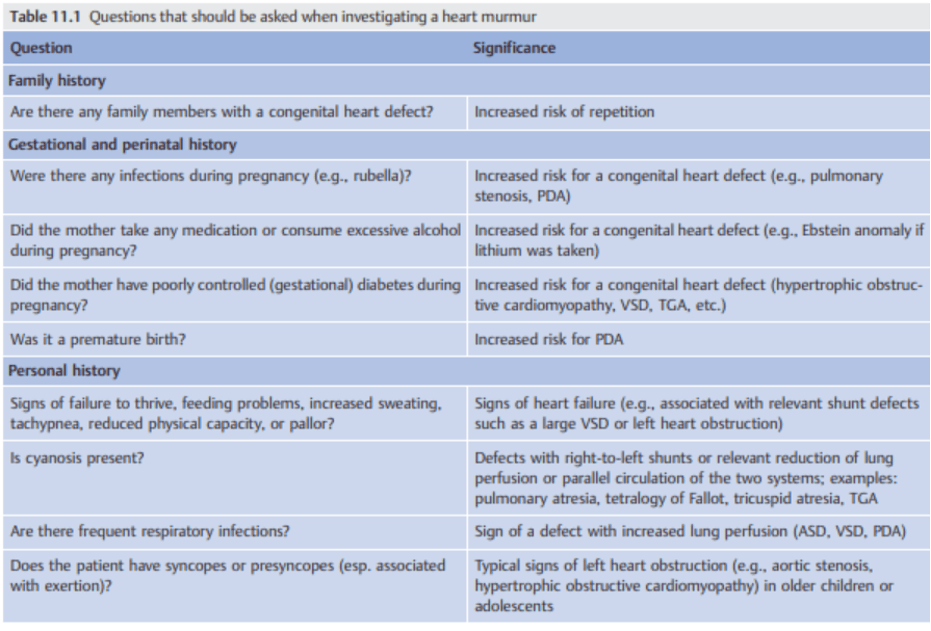
Family reports that the infant was born full term with no complications and was discharged home on the second day of life with mother. They were not told of a murmur being heard in the well baby nursery. The mother reports that the baby has been taking longer to feed over the last 1 week (had been taking 2 ounces of formula/feed, now it takes much longer).
Vital signs: Weight 4 kg (Birth weight 3.5 kg). Heart Rate 160 bpm, Respiratory Rate 54 bpm, Blood pressures (70/35 right arm, 72/33 right leg), saturations 100% on room air.
On exam the infant is nondysmorphic well appearing but there is mild increased work of breathing with subcostal retractions. The cardiac exam demonstrates a hyperdynamic precordium, regular rate and rhythm, normal S1, S2 and a harsh III/VI holosystolic murmur at the lower left sternal border. The abdomen is soft, the liver edge is 2 centimeters below the right costal margin. The extremities are warm and well perfused with 2+ brachial and femoral pulses bilaterally. The remainder of the infant exam is normal.
Important Questions:
- Birth history (prematurity? pulse ox screening?)
- Feeding history
- Tachypnea or increased WOB?
- Lethargy?
- Cyanosis?
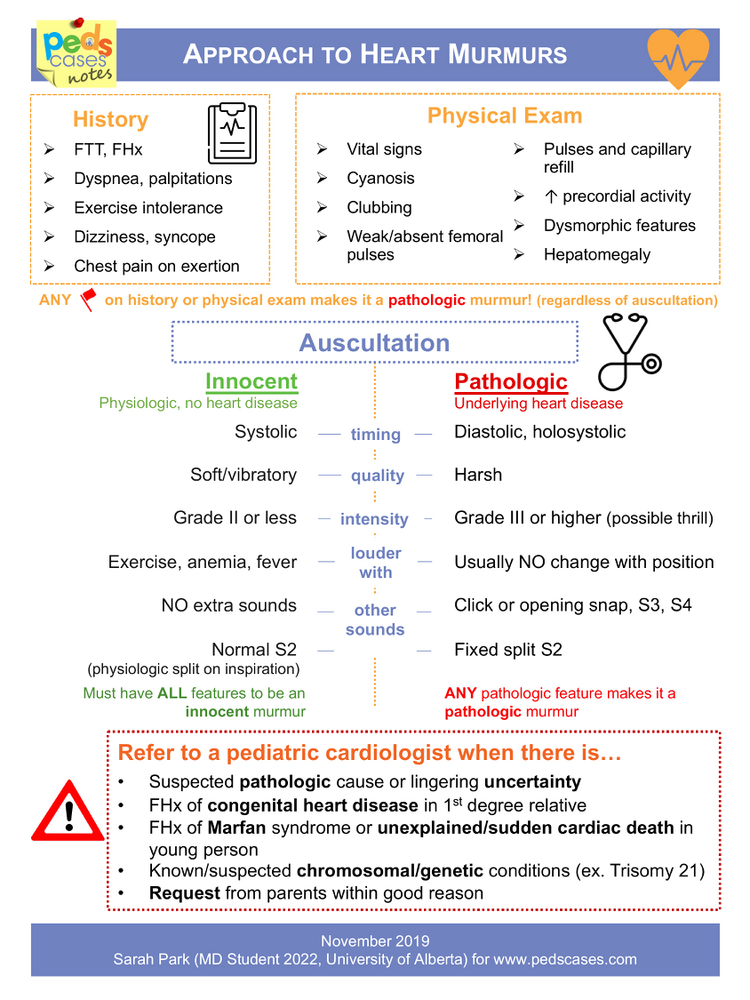
Key Components:
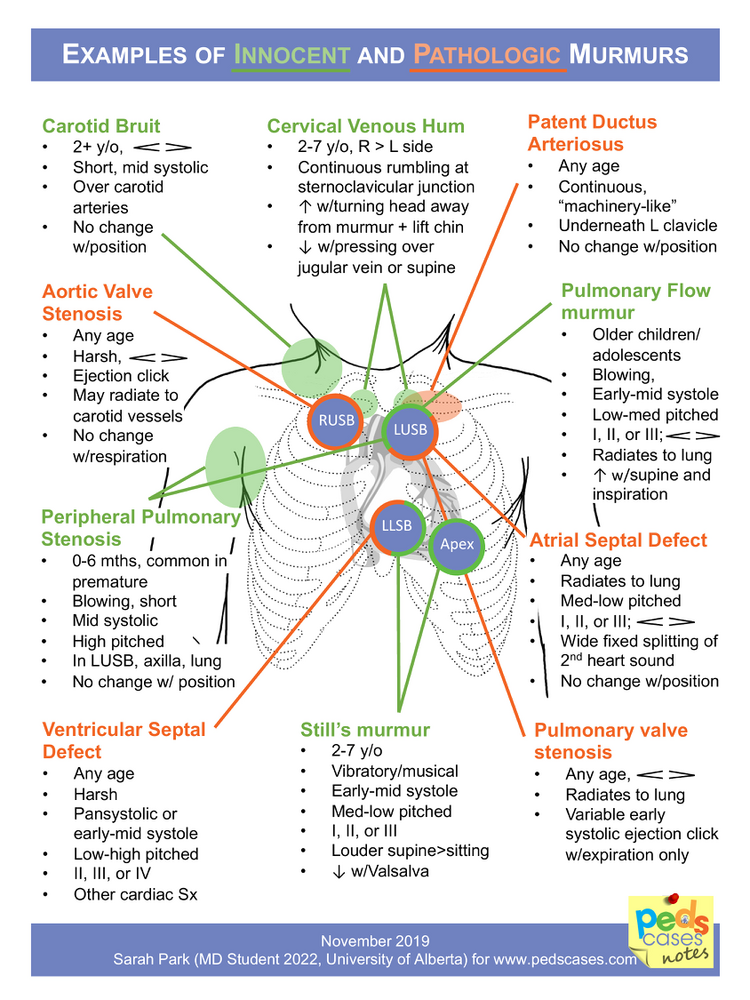
- Description of murmur
- Location
- Timing: Systolic/Diastolic
- Grading
- Pitch
- Importance of vital signs (weight trend), RR, HR, pulse ox, upper and lower ext BP
- Signs of infant heart failure: tachypnea, work of breathing, hepatomegaly, perfusion
- The PDA begins to close at 12-24 hours and fully closes at 2-3 weeks. Some neonates with “ductal-dependent” congenital heart disease require prostaglandin infusion to maintain pulmonary or systemic circulation until surgical or catheter intervention.
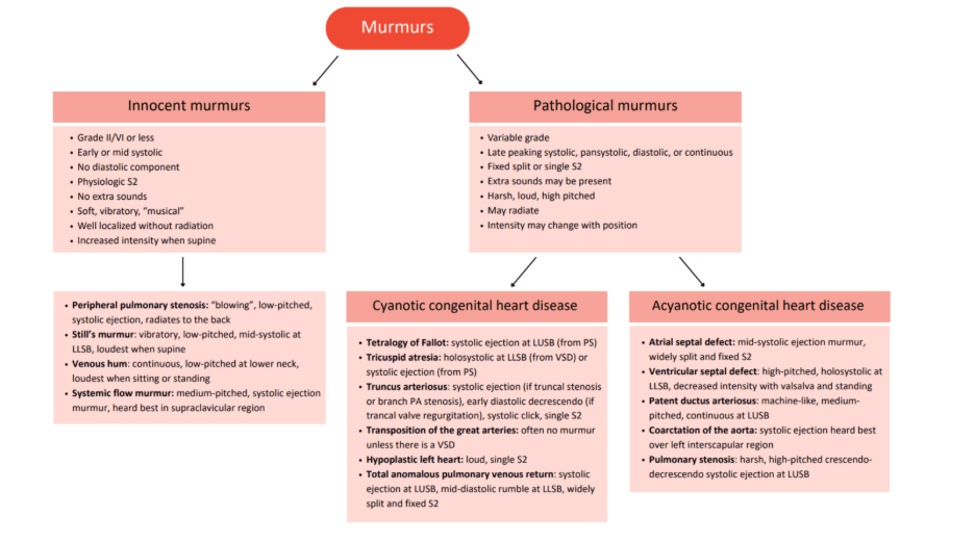
- The most common congenital heart disease is a VSD, followed by ASD. The most common cyanotic CHD is tetralogy of Fallot (TOF).
- Many CHDs are asymptomatic at birth. Symptoms may present in childhood or adulthood with cyanosis or symptoms of heart failure (shortness of breath, poor weight gain, and exercise/feeding intolerance [sweating with feeds]).
- Park’s Pediatric Cardiology for Practioners, 7th ed. 2021
- Chapter 2: Physical Examination
- Section on Auscultation and Heart Murmurs
- Chapter 2: Physical Examination
- Park’s pocket guide is a great student/resident resource to buy for those interested in Pediatric Cardiology
- Articles
- Videos
- Websites/Apps
- https://teachingheartauscultation.com/pediatric-murmur-recognition-program-intro (includes quiz with murmur audios)
- https://med.stanford.edu/content/dam/sm/peds/documents/Core%20Rotations/purple-team/PCU%20200%20Handbook%202018-19.pdf (from 2018 but good handbook)
- Heartpedia Mobile App
- CHOP OPEN Overview of Congenital Heart Disease Lecture by Dr. Dorfman (free to register)
- Podcasts

