Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC)
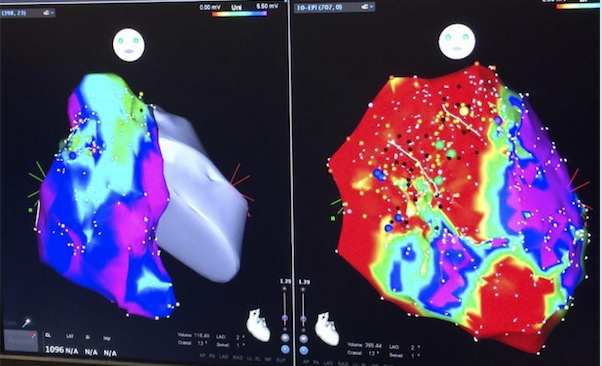
Arrhythmogenic right ventricular cardiomyopathy/dysplasia (ARVC/D) is primarily believed to be an inherited cardiomyopathy that subsequently results in significant myocardial fibrosis. The arrhythmogenic consequences that result from the development of fibrosis are similar to other types of cardiomyopathies, but the unique endocardial-epicardial disease process of ARVC/D requires a specialized approach for arrhythmia treatment in the electrophysiology laboratory. Although the association between ARVC/D and development of ventricular arrhythmias has become increasingly clear over the last 2 decades, our understanding of the arrhythmia mechanisms, underlying electrophysiologic substrate, and treatment strategies were significantly limited. Prospective studies performed in the electrophysiology laboratory by Penn EP faculty allowed detailed characterization and localization of abnormalities that cause ventricular tachycardia in these patients.
For many years catheter ablation was considered a limited and largely unsuccessful treatment for patients experiencing painful and recurrent defibrillator therapy. Through our increased understanding of the disease process, catheter ablation has evolved to become an effective and preferred therapy for a majority of these patients. We are actively continuing investigations to further understand the disease process and the necessary approaches to provide successful treatment.
Exciting firsts in Inherited Arrhythmogenic Right Ventricular Cardiomyopathy
Using our background of success in treating arrhythmias in patients with coronary artery disease, the Penn EP program has lead the field in the evaluation and treatment of patients with inherited arrhythmia disorders like ARVC.
In patients with ARVC Penn EP has been the first center to:
- Demonstrate the importance of epicardial (on the outside of the heart) ablation to eliminate ventricular tachycardia
- Demonstrate the absence of scar progression in most patients with ARVC - previously, it was thought to be a relentlessly progressive degenerative disease
- Describe excellent long-term outcomes with catheter ablation, including the elimination of the need for continued drug therapy
- Describe the common occurrence of atrial arrhythmias during long term follow-up after successful ventricular tachycardia elimination
- Describe unique ECG patterns on the 12 lead ECG that could characterize precise scar location before their procedure and want the opportunity
Our program has identified other exciting initiatives to create new “firsts” in the treatment of arrhythmias in patients with ARVC and other inherited arrhythmia syndromes that are part of active research investigations.

