2020 Media
- Dr. Roy Hamilton named as one of Cell's '1000 Inspiring Black Scientists'
- Dr. Roy Hamilton Presents at XII International Symposium on Neuromodulation
- Dr. Roy Hamilton Presents Keynote Address at ADRD Forum
- Michael Platt speaks about His New Book, "The Leader's Brain"
- Dr. Roy Hamilton discussed brainSTIM with the American Neurological Association (ANA)
- brainSTIM Director Dr. Roy Hamilton highlights the importance of the "#BlackInNeuro" Initiative
- Dr. Roy Hamilton shares presentation about his life and work in neurology with interns
- The brainSTIM Center's Grand Rounds Mini Symposium on Neuromodulation
- Utilizing Network Imaging to Personalizing and Optimizing Neuromodulation in Translational Cognitive Neuroscience
- This is Your Brain During a Pandemic
- Dr. John Medaglia chats with 1060 KYW about Zoom fatigue
- brainSTIM Core Faculty Member Flavia Vitale, PhD, interviewed by BBC World Service's Crowdscience podcast
- Center Highlight Archive
Dr. Roy Hamilton named as one of Cell's '1000 Inspiring Black Scientists'
 At the start of the year, brainSTIM Director Roy Hamilton MD, MS was named as one of the Cell Community of Scholars' '1000 Inspiring Black Scientists'. In the announcement, Cell emphasized the need to dispel the myth that Black scientists make up on a small percentage of those in the scientific community, and sough to highlight and amplify Black talent.
At the start of the year, brainSTIM Director Roy Hamilton MD, MS was named as one of the Cell Community of Scholars' '1000 Inspiring Black Scientists'. In the announcement, Cell emphasized the need to dispel the myth that Black scientists make up on a small percentage of those in the scientific community, and sough to highlight and amplify Black talent.
Additionally, Cell calls for an allocation of resources to further encourage young Black people to get involved with the sciences and in STEM fields, in order to continue to amplify Black voices and stop the obscuring of Black talent in scientific fields.
To read the full article and view the full list, click the link below.
Dr. Roy Hamilton Presents at XII International Symposium on Neuromodulation
 On November 9, PMC’s Dr. Roy Hamilton presented “Stimulating conversations: Using noninvasive neuromodulation to reveal and restore the language network” at the XII International Symposium on Neuromodulation. The event, hosted virtually from Sao Paulo, Brazil by Instituto SCALA, hosted talks from TMS and neuromodulators all over the world.
On November 9, PMC’s Dr. Roy Hamilton presented “Stimulating conversations: Using noninvasive neuromodulation to reveal and restore the language network” at the XII International Symposium on Neuromodulation. The event, hosted virtually from Sao Paulo, Brazil by Instituto SCALA, hosted talks from TMS and neuromodulators all over the world.
In his presentation, Dr. Hamilton discussed interhemispheric interactions in nonfluent aphasia, the use of TMS for post-stroke aphasia, as well as the use of tDCS for both post-stroke aphasia and neurodegenerative aphasias, before closing out by outlining some of the challenges and next steps for neuromodulation.
Dr. Hamilton laid out the processes of both past and current studies being conducted on the use of TMS for post-stroke aphasia, including those which showed improvements in the abilities of patients to name objects shown to them, as well as improvements in elicited speech. Additionally, he outlined studies examining the use of tDCS for primary progressive aphasia (PPA) in improving naming, spelling, and overall language performance in individuals, when compared to those receiving sham tDCS treatment.
Upon concluding his presentation, Dr. Hamilton addressed past insights achieved through past studies in neuromodulation, as well as current knowledge gaps and the next steps for improving study models, tools, and procedures in future neuromodulation studies.
Dr. Roy Hamilton Presents Keynote Address at ADRD Forum
 Racial Disparities and Inequalities in Early Detection, Diagnosis, and Treatment
Racial Disparities and Inequalities in Early Detection, Diagnosis, and Treatment
On November 5, the Pennsylvania Department of Aging hosted the 2020 Alzheimer’s Disease and Related Disorders Forum (ADRD), as attended virtually by both top researchers, clinicians, and stakeholders alike. Messages from Pennsylvania Governor Tom Wolf and Secretary of Aging Robert Torres were featured, in addition to a panel discussion between caregivers for those living with Alzheimer’s disease and other dementias, as well as an update from the Pennsylvania ADRD Task Force. The annual forum discussed racial disparities and inequities in early detection, diagnosis, and treatment, and emphasized the need for increased partnerships and support between medical establishments and communities of color, increased diversity amongst clinicians and investigators, and the need for increased awareness regarding the disproportionate impact of Alzheimer’s disease and related disorders on Latinx, African American, and Native American communities.
Roy Hamilton MD, MS, served as the forum’s keynote speaker. Dr. Hamilton began by giving a review of Alzheimer’s disease and its related disorders, including the difference between them, before moving on to addressing the disproportionate burden of Alzheimer’s disease in minorities, disparities of dementia care for people of color, and the steps that can be taken to address disparities and equity in AD.
When looking at statistics, rates of Alzheimer’s disease are more prevalent in minorities than amongst white populations. This is contributed to by a higher set of risk factors in people of color, including social determinants of health, bias and discrimination in medicine and disparities in research, cultural beliefs, and the impact of other diseases, such as hypertension or cardiovascular diseases, which can increase the risk of AD. This is also bolstered by cultural differences regarding the stigmas surrounding aging and mental decline in communities of color, which leads to seeking out care at a later stage of AD than white communities. Additionally, due to a lack of access to education on neurodegenerative diseases, lack of access to care, healthcare discrimination leading to higher care costs, medical racism and systemic inequality amongst health care systems, minorities in the United States receive inferior care for these disorders when compared to white populations.
“It is critical that we partner with communities of color comprehensively to enhance awareness of Alzheimer’s disease and promote diversity in research participants”, Hamilton said, emphasizing the need to build up trust between the medical community and communities of color after continual histories of medical racism, human rights violations, and unethical practices. As an example of successful endeavors into bolstering diversity amongst clinicians and researchers, Dr. Hamilton highlighted the Penn Memory Center’s own pipeline programs dedicated to increasing the number of scholars committed to the research and treatment of Alzheimer’s disease that come from diverse backgrounds and from communities of color.
Upon his conclusion, Dr. Hamilton reemphasized the increased prevalence and more severe symptoms of Alzheimer’s disease amongst communities of color due to social determinants of health, racial bias and discrimination in medical care, and differences in comorbid diseases. To address these factors, Dr. Hamilton stressed a need for effective efforts to address these disparities in care, including authentic community partnerships, workforce diversity, and ongoing cultural and bias trainings.
Michael Platt speaks about His New Book, "The Leader's Brain"
 brainSTIM Faculty Steering Committee member Michael Platt, PhD recently spoke with the Wharton School Press podcast about his new book, "The Leader's Brain: Enhance Your Leadership, Build Stronger Teams, Make Better Decisions, and Inspire Greater Innovation with Neuroscience", and how brain science can transform one's approach to leadership, team building, and marketing.
brainSTIM Faculty Steering Committee member Michael Platt, PhD recently spoke with the Wharton School Press podcast about his new book, "The Leader's Brain: Enhance Your Leadership, Build Stronger Teams, Make Better Decisions, and Inspire Greater Innovation with Neuroscience", and how brain science can transform one's approach to leadership, team building, and marketing.
As a James S. Riepe Penn Integrates Knowledge Professor of Marketing, Psychology, and Neuroscience, Dr. Platt has taken his extensive research into understanding how the human brain works, and has translated that into strategies that will help businesspeople get ahead in the workplace. When speaking with Wharton School Press, Dr. Platt details how his interdisciplinary work allows him to analyze business and leadership from a unique perspective.
"How can we use that information and the insights from these different disciplines...to address some of the biggest challenges facing business and facing society at large?" Dr. Platt questions, emphasizing the importance of bridging the gap between psychology, marketing, and neuroscience. Dr. Platt details some insights from his research that he has applied to his own work as a leader and director, and stresses the importance of those in leadership using their roles to connect with those they manage and create efficient and effective environments with high group morale.
When pondering the possible future intersections of neuroscience and business, Dr. Platt expresses excitement for the development of "critically important" wearable brain monitoring technologies, which will allow individuals to access and understand what goes on in their heads, and channel this information into improving their own performances.
Watch Dr. Platt's Full Interview With Wharton School Press Here
Dr. Roy Hamilton discussed brainSTIM with the American Neurological Association (ANA)
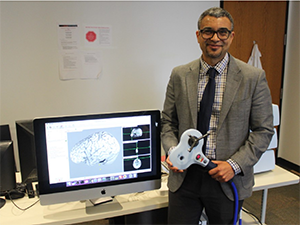 brainSTIM Director Dr. Roy Hamilton recently did a Q&A with the American Neurological Association, where he discusses all things brainSTIM, his work in noninvasive brain stimulation, and his relationship with the ANA.
brainSTIM Director Dr. Roy Hamilton recently did a Q&A with the American Neurological Association, where he discusses all things brainSTIM, his work in noninvasive brain stimulation, and his relationship with the ANA.
brainSTIM Director Dr. Roy Hamilton highlights the importance of the "#BlackInNeuro" Initiative
 In an interview with Penn Medicine News, brainSTIM Director Dr. Roy Hamilton highlights the importance of the "#BlackInNeuro" initiative, and emphasizes the need for increased diversity among faculty, post-docs, and students in neurology and its related fields.
In an interview with Penn Medicine News, brainSTIM Director Dr. Roy Hamilton highlights the importance of the "#BlackInNeuro" initiative, and emphasizes the need for increased diversity among faculty, post-docs, and students in neurology and its related fields.
Dr. Roy Hamilton shares presentation about his life and work in neurology with interns
 Dr. Roy Hamilton recently spoke about his life and work in neurology and neuromodulation in a presentation to members of the CTSA/ITMAT Internship Program. Watch the full presentation below.
Dr. Roy Hamilton recently spoke about his life and work in neurology and neuromodulation in a presentation to members of the CTSA/ITMAT Internship Program. Watch the full presentation below.
The brainSTIM Center's Grand Rounds Mini Symposium on Neuromodulation
 Check out the brainSTIM Center's Grand Rounds Mini Symposium on Neuromodulation, featuring core faculty members Desmond Oathes PhD, Flavia Vitale PhD, and John Medaglia PhD.
Check out the brainSTIM Center's Grand Rounds Mini Symposium on Neuromodulation, featuring core faculty members Desmond Oathes PhD, Flavia Vitale PhD, and John Medaglia PhD.
Utilizing Network Imaging to Personalizing and Optimizing Neuromodulation in Translational Cognitive Neuroscience
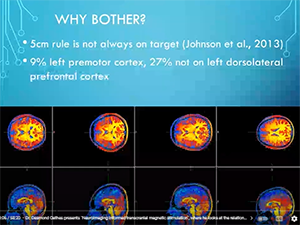
 brainSTIM Center core faculty members Desmond Oathes and John Medaglia both spoke at the NYC Neuromodulation 2020 Online Conference on April 22nd.
brainSTIM Center core faculty members Desmond Oathes and John Medaglia both spoke at the NYC Neuromodulation 2020 Online Conference on April 22nd.
Oathes and Medaglia spoke at a session chaired by Roy Hamilton entitled Utilizing Network Imaging to Personalizing and Optimizing Neuromodulation in Translational Cognitive Neuroscience, where they discussed the ever evolving understanding of how brain stimulation can target specific networks and circuits that underlie behavior. These advancements allow for the application of neuromodulation using increased precision on a specific individual level.
In Dr. Medaglia's talk, Integrating Network Anatomy and Function to Enhance Cognition with Neuromodulation, he emphasized how network anatomy varies across subjects, and can guide network function, cognition, and in turn can affect outcomes. He also discussed how person-centered network neuroscience can improve the prediction of neuromodulation outcomes and drive new neuromodulation practices.
Following Dr. Medaglia, Dr. Oathes presented Interleaved TMS/fMRI for casual mapping of cortical-subcortical connections toward novel personalized treatment targets. In this talk, Dr. Oathes explained his lab's motivation for pursuing a study which aims to improve the accuracy and individualization of clinical treatments when using rTMS to treat depression. He went on to discuss his lab's study into TMS targeting, which would improve accuracy in brain mapping in clinical treatment, as well as their foray into the search for pathways in the prefrontal cortex that would allow for deeper noninvasive modulation for treating anxiety and depression.
This is Your Brain During a Pandemic
 On NPR's The Pulse podcast, Roy Hamilton discusses the concept of at-home brain stimulation, and whether or not it's exactly a good idea.
On NPR's The Pulse podcast, Roy Hamilton discusses the concept of at-home brain stimulation, and whether or not it's exactly a good idea.
Dr. John Medaglia chats with 1060 KYW about Zoom fatigue
 How to stave off Zoom fatigue: Dr. John Medaglia talks with 1060 KYW about how to avoid video chat burnout.
How to stave off Zoom fatigue: Dr. John Medaglia talks with 1060 KYW about how to avoid video chat burnout.
brainSTIM Core Faculty Member Flavia Vitale, PhD, interviewed by BBC World Service's Crowdscience podcast
 Listen in on brainSTIM faculty member Flavia Vitale's interview with BBC World Service's Crowdscience podcast regarding novel materials for neuro-electronic interfaces.
Listen in on brainSTIM faculty member Flavia Vitale's interview with BBC World Service's Crowdscience podcast regarding novel materials for neuro-electronic interfaces.
Center Highlight Archive
December 2020 - Yvette Sheline, MD

The brainSTIM Center's monthly faculty highlight shines a spotlight on Yvette Sheline MD, MS, a McLure Professor of Psychiatry, Radiology and Neurology and the Director of the Center for Neuromodulation in Depression and Stress (CNDS), has spent thirty years in the field of neurology and neurophysiology.
Dr. Sheline’s research interests revolve around using neuroimaging techniques to determine how depression affects the brain and to understand how stress produces functional dysregulation. She also investigates the treatment effects of antidepressants and cognitive behavioral therapy (CBT) on patients with depression, anxiety, and PTSD, and seeks to understand the brain mechanisms of treatment effects and plasticity across disorders.
After receiving her BA in Biology from Harvard University, Dr. Sheline obtained her MS in Neurophysiology from Yale University, before going on to attend medical school at Boston University. At the end of her psychiatry residency, Dr. Sheline worked in emergency psychiatry and public mental health, before returning to her interest in clinical neuroscience upon joining the faculty at Washington University Medical School. She joined a lab conducting neuroimaging analysis and began to conduct research on structural brain differences in depression. Specifically, Dr. Sheline examined hippocampal volume in depressed individuals compared to controls, how hippocampal volume loss progressed in relation to continued untreated depression, and how antidepressant treatment protected against hippocampal volume loss in depressed patients. This work would help bring about the acceptance of depression and disorders like it as brain illnesses, instead of functional illnesses. Additionally, her work examined other associated features of depression, including vascular risk factors and neuropsychological profiles.
With her recruitment to the University of Pennsylvania as the Director of the University of Pennsylvania’s Center for Neuromodulation in Depression and Stress (CNDS), Dr. Sheline wanted to focus on improving treatments for depression and related conditions by working to better understand how existing treatments work in the brain. Dr. Sheline has used neuroimaging as a means to further this mission, examining brain changes resulting from neuromodulation with antidepressants, cognitive behavioral therapy and TMS.
At the Center for Neuromodulation in Depression and Stress (CNDS), researchers are currently working to augment cognitive behavioral therapy (CBT) with computer exercises to produce changes in cognitive control networks, seen in task-evoked fMRI brain activity and resting state fMRI connectivity in order to examine the relationship to treatment responses. Additionally, researchers at CNDS are examining the use of real time fMRI feedback in reducing depression, as well as in examining and monitoring symptoms and defining biotypes across individuals.
When looking to the future of research efforts at CNDS and at the University of Pennsylvania, Dr. Sheline hopes to see more studies using individualization in TMS targeting to improve treatment outcomes and with collaborators, more studies probing TMS mechanisms. By improving targeting techniques, neuromodulators would then be able to create more individualized and effective treatments for patients, and in turn elevate patients care and quality of life.
Dr. Sheline also has a positive view of the opportunities for researching TMS techniques and treatments as a part of the brainSTIM Center. She endorses the potential for collaboration amongst faculty members who work across a variety of disorders, which could allow for a further understanding of the commonalities of TMS properties for people suffering from disorders relating to stroke, for example as well as individuals suffering from PTSD, depression, and anxiety.
Learn More About the CNDS Here
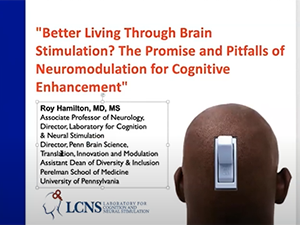
October 2020 - Branch Coslett, MD
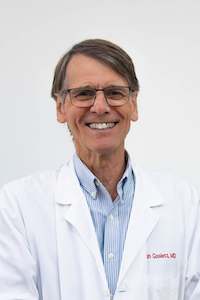 Every month, the brainSTIM Center shines a light on the exciting research and work our core faculty have been doing both inside and outside of their labs and practices. This month’s highlight features H. Branch Coslett MD, a William N. Kelley Professor of Neurology at the Center for Cognitive Neuroscience at the University of Pennsylvania, Research Neurologist at the Moss Rehabilitation Hospital, and Co-Director of the University of Pennsylvania’s Laboratory for Cognition and Neural Stimulation (LCNS).
Every month, the brainSTIM Center shines a light on the exciting research and work our core faculty have been doing both inside and outside of their labs and practices. This month’s highlight features H. Branch Coslett MD, a William N. Kelley Professor of Neurology at the Center for Cognitive Neuroscience at the University of Pennsylvania, Research Neurologist at the Moss Rehabilitation Hospital, and Co-Director of the University of Pennsylvania’s Laboratory for Cognition and Neural Stimulation (LCNS).
Having spent forty years in the field of neurology, Dr. Coslett’s research interests include behavioral and cognitive neurology, as well as understanding the bases for human cognition through the study of human spatial cognition, functional imaging, and transcranial magnetic stimulation.
After receiving his MD from the University of Pennsylvania, Dr. Coslett completed his residency in 1981 at the University of Virginia. Upon meeting his mentor, Ken Heilman, Dr. Coslett became interested in cognitive behavioral neurology and completed his fellowship at the University of Florida in 1983. His first experience with TMS came in an effort to address the question of the role of the right hemisphere in reading. Specifically, he examined the right hemisphere’s role in the reading of a patient with pure alexia, a condition in which patients can see individual letters, but not full words. Coslett and his fellow contributors used a first generation TMS coil to disrupt reading in patients, and found that the application of TMS to the right hemisphere disrupted patient's reading, whereas reading was not disrupted by TMS when applied to the left hemisphere.
Coslett employs TMS as an experimental approach in neurology, and emphasizes its usefulness when used in conjunction with traditional methods in cognitive neuroscience investigations. He cites TMS and tDCS as promising approaches when paired with therapies, especially in patients with brain lesions. Currently, the LCNS is conducting a five-year NIH-funded study of TMS in conjunction with speech therapy to treat chronic aphasia in approved patients with six or more months of aphasia due to stroke. Groups in the study all receive speech therapy, but are separated into cohorts which, in addition to therapy, receive either real or sham (i.e. placebo) TMS treatment. Language performance is assessed before and six months after treatment in order to assess the efficacy of stimulation.
Dr. Coslett hopes to use the results of this study to improve the care of aphasia, a debilitating chronic condition. Upon looking back on his years in the field, Coslett emphasizes how far treatment methods have come. When he initially became interested in behavioral neurology, the field was largely a diagnostic endeavor, with very little in the way of applied treatment options. However, many areas of neurology have seen huge advancements. For example, there are now effective treatments for a range of autoimmune and immune-mediated conditions, where before there was limited understanding of the conditions. Furthermore, the use of CT scans and MRIs, as well as other imaging techniques have revolutionized the understanding of many neurologic conditions, including stroke and neurodegenerative disorders.
When looking to the future, Dr. Coslett emphasizes promising new developments, pointing to an emerging molecular genetics revolution. He believes that researchers will soon be able to identify, understand, and modify genetic defects or differences that are linked to neurological conditions and may modify the response to noninvasive brain stimulation. This may also allow researchers to better understand or predict patient response to treatment modalities such as TMS and tDCS.
Dr. Coslett hopes to continue to innovate and elevate the field of neurology through his work with the brainSTIM Center, and in using brain stimulation for therapeutic and scientific purposes. By continuing his search for answers to outstanding questions in cognitive neuroscience, Dr. Coslett aims to create individualized and effective treatment approaches for patients with a variety of conditions. In collaboration with other investigators at the brainSTIM Center, Coslett hopes to advance the use of novel treatments to research, repair, and enhance human brain function.
Learn More About the LCNS Here
August/September 2020 - Mario Cristancho, PhD

The brainSTIM Center is pleased to highlight the work of Dr. Mario Cristancho MD, is an Assistant Professor of Clinical Psychiatry at the University of Pennsylvania, Director of Penn's Transcranial Magnetic Stimulation and Neuromodulation Program, Director of the Outpatient Psychiatry Services' Electroconvulsive Therapy (ECT) Treatment Program at the University of Pennsylvania and Neuromodulation Service Clinician in the University of Pennsylvania’s Department of Psychiatry. Additionally, Dr. Cristancho serves as an Attending Physician at the Hospital of the University of Pennsylvania, and as a clinician at the Comprehensive Consultation Service Mood Disorders Treatment Center at the University of Pennsylvania.
Having been in practice for almost a decade, Dr. Cristancho’s area of specialization is the treatment of anxiety disorders and mood disorders, including depression, bipolar disorder, and major depressive disorder. Dr. Cristancho works with many tools to treat patients, including transcranial magnetic stimulation (TMS), vague nerve stimulation (VNS), electroconvulsive therapy (ECT), and deep brain stimulation (DBS).
Dr. Cristancho’s work in neuromodulation draws attention to the need for individualized therapies in the care of patients with treatment-resistant mood disorders. Since Dr. Cristancho usually sees patients who have already tried more than one approach to treating their respective disorder(s),he usually uses psychotherapy in addition to medication to jumpstart response and decrease the chance of relapse. He also uses neuromodulation to get patients out of severe depressive states, in order to get them to a place where they may begin to respond to medication or more traditional treatments.
In addition to his clinical work, Dr. Cristancho has been collaborating with fellow brainSTIM core faculty members Desmond Oathes, PhD, and Yvette Sheline, PhD, to improve TMS targeting, accuracy, and depth of treatment, as well as the individualization of treatment. This both changes the way TMS is used, and allows Dr. Cristancho to apply these research findings directly to patients. Together, they have modified ECT and TMS in order target stimulation more effectively, at a faster pace, and at a deeper level, and have changed how they can stimulate in terms of frequency in relation to symptoms exhibited. Additionally, they have made these modifications whilst lessening cognitive effects from its original version.
Dr. Cristancho hopes to use research findings and subsequent trials to advance the widespread use of novel treatments, and to one day enable access to neuromodulation for every patient who needs it. He hopes that as a part of the brainSTIM community, the Center’s faculty can work together to elevate patient care, treatment, and access to these life changing treatments.
July 2020 - Michael Platt, PhD
 The brainSTIM Center would like to highlight Michael Platt, PhD, James S. Riepe Penn Integrates Knowledge University Professor of Marketing, Psychology, and Neuroscience, and Director of the Wharton Neuroscience Initiative at the University of Pennsylvania.
The brainSTIM Center would like to highlight Michael Platt, PhD, James S. Riepe Penn Integrates Knowledge University Professor of Marketing, Psychology, and Neuroscience, and Director of the Wharton Neuroscience Initiative at the University of Pennsylvania.
Dr. Michael Platt's principal research interests primarily focus on the underlying biological mechanisms that govern decision making in social environments, and how to translate this knowledge into not only how to make oneself into a better leader and team player in professional environments, but also into treatments for those with social disorders.
Dr. Platt holds both a BA in biological anthropology from Yale and a PhD from Penn in biological anthropology. His work goes beyond traditional anthropology, and envelops neuroscience, economics, marketing, and psychology. This can particularly be seen in his work with the Wharton Neuroscience Initiative, where he translates the study of neuroscience to create groundbreaking business strategies and leadership techniques. Dr. Platt’s work is frequently featured in the media, where he has been recognized by the New York Times, The Wall Street Journal, NPR, ABC, BBC, and HBO Vice.
Dr. Platt has multiple new and exciting projects going on at his laboratories, two different technologies that were spotlighted in particular. In one project, Platt’s lab is developing high fidelity, high quality, reliable, and comfortable EEG devices that can be used to enhance patient care, whilst achieving more accurate readings. These EEGs can also be used to optimize not only work in office settings, but can optimize performance in decision making on the part of coaches in sports. His lab is also putting efforts into work with optogenetics in human and non-human primates to confront neurobiological problems. By using microLED systems developed in collaboration with fellow brainSTIM Core Faculty member Dr. Flavia Vitale, Dr. Platt and his researchers have found the possibility of illuminating different parts of the brain noninvasively and wirelessly, in order to stop seizures in epilepsy or shuts off schizophrenic episodes by modulating activity in different areas of the human brain.
Dr. Platt’s work with nonhuman primates has also shed light on how the human brain is effected by both genetic and environmental factors that influence both their place in their respective environments, but also social behaviors and disorders. Since the brains of humans and monkeys are so similar, researchers have studied monkeys found to have similar genetic makeups that, like humans, predispose them to specific disorders such as social anxiety or autism. There is a considerable amount of symptom overlap between monkeys and humans when it comes to behavioral or social disorders, which allows researchers to study and better understand the biological origin of these disorders in humans. Dr. Platt heavily focuses on the social structures of monkeys in their environments, and how this can be translated to the human condition. After the destruction caused by Hurricane Maria to Cayo Santiago Island in Puerto Rico, where researchers had been studied the behaviors of monkeys for 80 years already, the responses of monkeys to environmental variables, like a lack of food, shade, and water, differed greatly depending on the social environments they existed in. Researchers saw that in response to stressful events like a hurricane, monkeys were drawn to creating more social connections and alliances to support one another. The monkeys who were more isolated or lacked a strong social structure, did not react as well to destruction wrought by the hurricane.
These responses are telling in the human world as well. On a personal level, these findings could indicate that people react and handle traumatic events more effectively and in a healthier manner if they have a good social support structure around them. In a professional environment, these findings might indicate that employees might be better able to handle stress if their company emphasized teamwork and fostered a sense of belonging at an establishment, employees would be more resilient when faced with challenging or stressful situations, and would lean on one another for support, instead of taking that stress and negativity home with them.
Through studying the social and psychological behaviors of monkeys, Dr. Platt and his lab translate this into the human world, in both a social and professional sense. These ideas are merged in Dr. Platt’s work as Director of the Wharton Neuroscience Initiative, which exists at the intersection of neuroscience and business. The Initiative emphasizes the deeper neurological factors that can be tapped into to create better working environments, recruitment strategies, brand management, and market targeting. The program, which recently received an anonymous $10 million donation, seeks to use this generous gift to expand their work in this field, extend further research opportunities to faculty, MBA and graduate students, in addition to creating summer programs, and deepening partnerships with various schools and programs across the University of Pennsylvania.
Dr. Platt’s work across the University (and the world!), has allowed him to study and work in many fields that are of interest to the brainSTIM Center. In addition to his work in neurobiology, psychology, and marketing, Dr. Platt has a concerted interest in using stimulation to study brain activity and function, and in turn using this to treat human behavioral disorders and enhance human brain function. Beyond this, he and his researcher team seeks to use brain stimulation to further delve into how the stimulation itself alters brain function and activity. His work only fosters further collaboration throughout the Center, and enriches the field of neuromodulation as a whole. We are excited to have the chance to have Dr. Platt as a core member of the Penn brainSTIM faculty, and cannot wait to see what he does in the future.
Learn More About The Wharton Neuroscience Initiative
June 2020 - Flavia Vitale, PhD
 The brainSTIM Center highlights the work of faculty member Flavia Vitale PhD, Assistant Professor of Neurology and Physical Medicine and Rehabilitation at the University of Pennsylvania, and director of Penn’s Vitale Lab. Her principal research interests revolve around using and developing flexible bioelectronic and nanostructured materials and devices for high resolution, minimally invasive recording and stimulation of neurological and neuromuscular activity.
The brainSTIM Center highlights the work of faculty member Flavia Vitale PhD, Assistant Professor of Neurology and Physical Medicine and Rehabilitation at the University of Pennsylvania, and director of Penn’s Vitale Lab. Her principal research interests revolve around using and developing flexible bioelectronic and nanostructured materials and devices for high resolution, minimally invasive recording and stimulation of neurological and neuromuscular activity.
A native of Rome, Italy, Dr. Vitale earned her B.S. and M.S. in Biomedical Engineering at the Università Campus Biomedico di Roma in 2008. In 2012, she received her Ph.D. in Chemical Engineering at the Università di Roma. She then worked on high-performance biomateirals and bioelectronic interfaces based on carbon nanomaterials whilst completing her postdoctoral training at Rice University. This was followed by neuroengineering research training in the Penn Center for Neuroengineering and Therapeutics.
Some of the most exciting innovations emerging from the Vitale lab involve the use of Ti3C2 MXene for bioelectronics. First discovered in 2011, MXenes are a family of atomically thin, two-dimensional compounds that have shown great promise for use in electrochemical and electronic devices. Ti3C2 MXene possesses a number of remarkable properties that make it superior to materials that are currently used to monitor and modulate brain activity. Researchers in Dr. Vitale’s lab have used Ti3C2 MXene to create implantable microelectrode arrays. These flexible, highly conductive, nonmetallic/nonmagnetic, tiny arrays can be used intracranially to collect high-fidelity data and are much more biocompatible than conventional, inflexible materials. More information about the fabrication of Ti3C2 MXene microelectrode arrays can be found below. To listen to Dr. Vitale's interview with the BBC World Service's Crowdscience podcast regarding novel materials for neuroelectronic interfaces, follow the link provided.
Dr. Vitale’s work is of considerable interest to the neuromodulation community at Penn and beyond, especially since she is also developing noninvasive applications for these remarkable nanomaterials. Currently working with fellow brainSTIM faculty member John Medaglia, Dr. Vitale is exploring whether Ti3C2 MXene can be used to develop the next generation of electrodes for use in surface electroencephalography (EEG). By creating better tools for monitoring brain activity, clinicians and neuroscientists can better understand the physiologic effects of neuromodulation. Moreover, the development of superior electrodes may be promising for investigators who employ transcranial electrical stimulation (tES) and related neuromodulation technologies that use deliver brain stimulation via electrodes.
When asked about the ‘big picture’ goals of her research, Dr. Vitale stresses that her mission to translate the results and findings of her work into the development and use of technologies and devices that will directly translate into the advancement of patient care and outcomes. We’re extremely excited to have the opportunity to work with Dr. Vitale as a core faculty member of the Penn brainSTIM Center.
Learn More About Ti3C2 MXene Microelectrode Arrays
Listen to Dr. Vitale's Crowdscience Interview Here

