Archived News
2023
Nov 23
Autoimmune disease
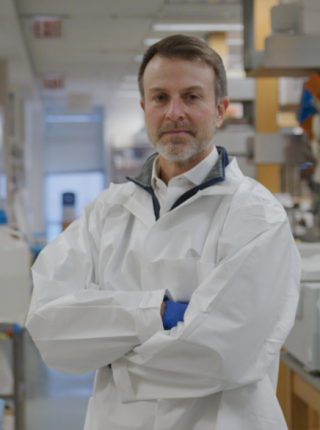
A research team led by Michael Mitchell of the School of Engineering and Applied Science has developed a lipid nanoparticle platform to deliver Foxp3 mRNA to T cells for applications in autoimmunity. “Broadly, this platform can be used to engineer adoptive cell therapies for specific autoimmune diseases and can potentially be used to create therapeutic avenues for allergies, organ transplantation, and beyond,” Mitchell says.
Sept 2023
Penn Opens New Multi-Disciplinary Research Labs in One uCity Square

Drew Weissman, MD, PhD, the Roberts Family Professor in Vaccine Research in Infectious Diseases, Harvey Friedman, MD, a professor of Infectious Diseases, and Vladimir Muzykantov, MD, PhD, Founders Professor in Nanoparticle Research, are among a group of prominent Penn scientists moving to new lab space in the 13-story One uCity Square building in West Philadelphia. The move consolidates research on messenger RNA, nanoparticles, and other cutting-edge biomedical technology.
When Is the Best Time to Get Your Flu, COVID-19 and RSV Shots?

Fall brings more than a chill in the air and changing leaves: it also ushers in respiratory virus season. E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics, shared insights into timing vaccines to stay protected, such as for the flu. For example, if you get sick with the flu before you’ve been vaccinated, you should still get the vaccine about a month later, because the flu vaccine typically protects against four types or strains of influenza.
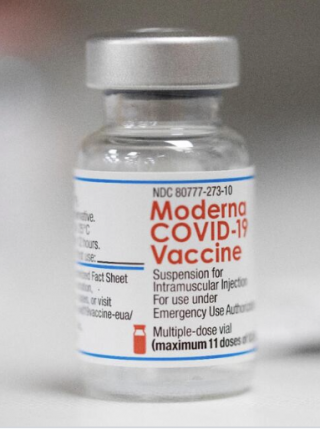
Updated COVID-19 Vaccine Rolling Out to Pharmacies Nationwide

The updated COVID-19 vaccine, approved recently by the FDA, debuted this week. E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics, spoke about the vaccine and noted that those receiving the new booster should expect “at least some coverage of a lot of the variants that may arise over the next four to six months.”
July 2023
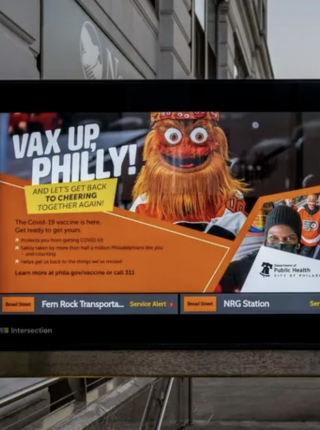
No, COVID Vaccines Don’t Contain Nanotechnology That Can Be Programmed via 5G Wireless Networks
E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics, helps to disprove a rumor that COVID-19 vaccines can be controlled wirelessly via “lipid nanoparticles” in the vaccine, including ones with a “cationic,” or positive, charge. “These charges are very simple, completely normal, chemistry,” Wherry said. "Nothing at all nefarious about this.”
May 2023
CRISPR Delivery Method Offers Gentler Approach to Editing T Cells

Research findings published in Nature Biotechnology outlined the development of a new gene editing technique which could help produce cell-based therapies. Senior author E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics, discussed the results. “The biggest advantage is that we can edit really fragile cells. We get super-high viability and really efficient editing in cells that would otherwise die when you try to edit them.”
Genome Web • Penn Medicine News Release
April 2023
Using Virus’ Lock-Pick Skills for Good

By borrowing protein fragments that viruses use to get into the body’s cells, scientists may be able to boost the efficiency and effectiveness of gene-editing techniques, with an eye toward super-charging cell therapies for cancer and other conditions. The team of researchers co-led by E. John Wherry, PhD, the Richard and Barbara Schiffrin President’s Distinguished Professor and Chair of the Department of Systems Pharmacology & Translational Therapeutics, believe that this “theft” from bad-actor viruses could also speed up the creation of better lab models for scientific study.
Researchers Identify Resistance Mechanism in Prostate Cancer
A particularly tough form of prostate cancer reboots tumor growth after treatment with the help of a testosterone-synthesizing enzyme called AKR1C3, according to a Penn Medicine research team including Andrea Detlefsen, a predoctoral fellow, and Trevor Penning, PhD, the Thelma Brown and Henry Charles Molinoff Professor of Pharmacology. This discovery opens up a potential new target for future treatments to pierce particularly resistant prostate cancers’ defense mechanisms.
Feb 2023
The Case of the Incredibly Long-Lived Mouse Cells
Scientists kept rodents’ immune T cells active four times longer than mice can live — which has huge implications for cancer, vaccination, and aging research. “It’s probably one of the most extraordinary papers in immunology that I’ve seen, easily in the past decade,” said E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics, who was not involved in the study. “It tells us that immunity can be incredibly durable, if we understand how to generate it properly.”
Jan 2023
Five things to know about this year’s ‘tripledemic’
Flu season came early this year, RSV reared its ugly head, and now there’s a new SARS-CoV-2 variant circulating. Immunologist E. John Wherry and influenza expert Scott Hensley of the Perelman School of Medicine spoke with Penn Today about what this confluence means for our immune systems, vaccinations, and viral competition.
What Is COVID Actually Doing to Our Immune Systems?
A new idea about how COVID-19 can affect immunity has emerged: that even mild infections routinely cause consequential damage to our bodies’ defenses. However, robust longitudinal data starting prior to the pandemic would show “whether we’ve seen large-scale changes in immune fitness,” said E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics, and we just don’t have it. In its absence, “the evidence of a long-term impact on the immune system in fully recovered COVID-19 patients, whether mild or severe, is really pretty thin.”
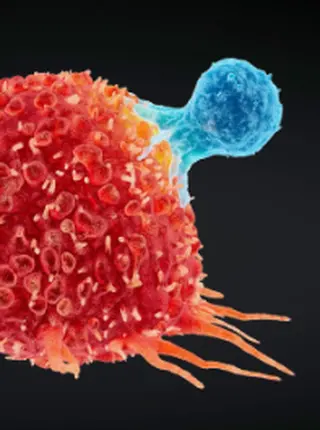
The race to supercharge cancer-fighting T cells
Advances in genome editing through processes such as CRISPR, and the ability to rewire cells through synthetic biology, have led to increasingly elaborate approaches for modifying and supercharging T cells for therapy. Avery Posey, PhD, an assistant professor of Pharmacology, and Carl June, MD, the Richard W. Vague Professor in Immunotherapy, explain how new techniques are providing tools to counter some of the limitations of current CAR T cell therapies.
2022
Sept 2022
Back to School

As children start returning to school, COVID-19 and monkeypox are still concerns. The Perelman School of Medicine’s E. John Wherry and Jennifer Brady offer suggestions to make the transition back to school easier while also allowing families to prioritize their health and well-being.
The Big Booster Question We Should Be Focused On

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, co-wrote a piece examining the state of vaccine protection today and future booster policy. “Anyone who would benefit from an additional boost should act as soon as one is authorized for their age- and health-risk group. If that’s the current standard vaccine, take it, and don’t wait for an omicron-based one,” the authors noted. “When those BA.4/5-based vaccines are rolled out, wait a sensible time (multiple months) before having another boost.”
August 2022
Am I Going to Get COVID-19 Again? What to Know About Reinfection.
Even with the newer COVID-19 variants, the vaccines still protect against severe disease. However, variants may continue to evolve to be more effective at getting through the body’s initial line of immune defense. For now, that likely means regular booster shots will be recommended, explained E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology.
Philadelphia Inquirer • Philadelphia Inquirer (2)
July 2022
As BA.5 Spreads, How Long Will a Prior COVID-19 Infection Protect You?

Experts say the window between infections might be shrinking, fueled in part by the immune-evading omicron BA.5 subvariant, although researchers are still gathering data. A COVID-19 infection is no longer a “get out of having COVID” card for the next three months. “I don’t think anyone should think they’re invincible,” explained E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology.
A Better Way to Measure Immunity in Children

Scientists have argued that COVID-19 vaccine manufacturers should have been measuring T cells, which can kill infected cells and rid the body of the virus. That “would have allowed us to possibly make a different decision about allowing a vaccine to move forward earlier,” said E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology. “If we don’t measure the T cells, we’re missing a big part of what’s happening.”
New York Times • New York Times (2)
U.S. Grapples With Whether to Modify COVID-19 Vaccine for Fall
Health authorities are facing a critical decision: whether to offer new COVID-19 booster shots this fall that are modified to better match the latest changes of the coronavirus. The top candidates are “bivalent” shots — a combination of the original vaccine plus omicron protection. That’s because the original vaccines do spur production of some virus-fighting antibodies strong enough to cross-react with newer mutants — in addition to their proven benefits against severe disease, explained E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology.
June 2022
Novavax Hopes its COVID Shot Wins Over FDA, Vaccine Holdouts

Novavax is waiting for FDA approval on its mRNA vaccine which is a more generic vaccine compared to the mRNA COVID vaccines. The company thinks that some people will be more comfortable with their vaccine since it's a protein vaccine designed like most of the other vaccines people receive. E. John Wherry, PhD, chair of Systems Pharmacology & Translational Therapeutics, said that, with the data so far, the Novavax vaccine appears to be an "impressive protein vaccine."
The U.S. Is About to Make a Big Gamble on Our Next COVID-19 Winter

Experts are expected to choose a vaccine recipe for the fall, when omicron may or may not still be the globe’s dominant variant. Commenting on a potential omicron-only vaccine, E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, was one of several scientists who said it would be safer to keep something with the original variant.
A Silver Lining for Those Who Have Been Infected by Omicron

People who are vaccinated and then get infected with omicron may be primed to overcome a broad range of coronavirus variants, judging from early research. “We should think about breakthrough infections as essentially equivalent to another dose of vaccine,” explained E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology.
Should Parents Wait to Get the COVID-19 Booster for Their Children?

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, answered questions after the FDA authorized COVID-19 boosters for kids ages 5-11. “This is great news,” Wherry said. “About 1,000 kids have died from COVID-19 over the pandemic, so kids are really at risk.” He also discussed the amount of disinformation out there on vaccines, which has contributed to vaccine hesitancy.
The Search for Longer-lasting COVID-19 Vaccines

There are still many questions left to answer about COVID-19 vaccines and immunology, said E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology. Those questions include: How long do memory B cells and memory T cells last? Why do different people respond differently to these vaccines? “These and many more questions still need answers if we are going to use this platform most effectively,” Wherry noted.
Epigenome Editing Decreases Alcohol Seeking and Anxiety in Rats

Elizabeth A. Heller, PhD, an assistant professor in Systems Pharmacology & Translational Therapeutics, commented on a study which found that a CRISPR-based system that reversed epigenetic changes caused by adolescent binge drinking reduced adult addiction-like behaviors in rats. Heller said that while a lot of work needs to be done before a CRISPR-based treatment could be approved for people, the fact that the authors delivered the CRISPR-based treatment in adulthood is particularly encouraging.
May 2022
What Does ‘Protection’ Against COVID-19 Really Mean?

Last month, E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, along with researchers, physicians, and biotech representatives sent a letter to the FDA urging the agency to monitor T cells — alongside antibody levels — to better assess immunity to determine the effectiveness of new vaccines undergoing review by regulators. Wherry spoke with Scientific Americanabout T cell measurement and why it is important for vaccine studies.
It Feels Like Everyone Is Non-COVID Sick Right Now. What Gives?
E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, was quoted discussing how the immune system works and how babies’ immune systems differ from adult ones. “Your immune system has layers to it,” Wherry said. “Think about it a bit like LEGO blocks.”
Finding the Genetic Links Behind Drug Addiction

Elizabeth Heller, PhD, an assistant professor of Pharmacology and head of a lab of Neuroepigenetics, focuses on studying molecular brain mechanisms, aiming to uncover chronic changes that can happen and keep happening in the brain long after exposure to addictive substances ends.
Heller’s dedication to basic science is matched only by her commitment to colleagues, her students, and those who may one day benefit from breakthroughs made in her lab. In a recent Q&A, she discussed finding a love of neurology, her unique research, and running a neuroscience lab throughout the pandemic.
Read the full Faculty Q&A on the Penn Medicine News Blog →
Uncovering Insights into Cellular Processes

Two recent studies led by Vera Moiseenkova-Bell, PhD, a professor of Pharmacology, outline a better understanding of how transient receptor potential vanilloid (TRPV) channels — which impact a range of cellular processes, from pain sensation to cancer — work in cells at the molecular level. Results outlined in a Cell Reports paper gave insights into the mechanisms of TRPV5 — a calcium-selective ion channel only found in the kidney — which could be helpful in development of therapeutics for kidney stone disease. In addition, findings featured in a Nature Communications article focus on the TRPV2 ion channel, which have recently been found to play a role in a variety of cancers. Moiseenkova-Bell and team discovered a drug binding site which may help drug design tied to TRPV2-related cancer growth.
Read the paper in Cell Reports →
U.S. May Default to Annual COVID-19 Boosters Without Sufficient Data
Last week experts signed a letter urging the FDA to put more emphasis on assessing additional parts of the immune response to COVID-19 vaccines, arguing that measuring T cells is critical to understanding long-lasting vaccine protection. “I think there are a lot of forces here that have had us almost myopically assessing antibodies as the guiding force in what immune measurements are most important,” said E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, one of the letter writers. “The antibody trajectories don’t explain the fact that nobody’s ending up in the hospital.”
Scientists Urge FDA to Assess T-Cell Levels In COVID-19 Vaccine Analysis

More than 60 scientists from across the United States have signed a letter to the Food and Drug Administration asking the agency to include T cells as a measurement of effectiveness for COVID-19 vaccines, instead of just looking at antibodies. While antibodies protect against initial infection, T-cells protect against hospitalization, explained E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, one of the letter writers.
Inside Health Policy • Boston Globe • Biospace
Should You Get Another COVID-19 Booster, if Eligible?

The FDA has authorized additional COVID-19 shots for older Americans and those with certain immune deficiencies. E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Institute for Immunology, spoke about the news to a wide variety of media outlets, including the Associated Press, CBS News, and The Atlantic, among others. “I’m a firm believer in vaccines. I like the idea of physicians and immunocompromised and high-risk patients having options,” Wherry told the New York Times. WHYY also highlighted findings from a recent Cell study by Wherry and colleagues that demonstrated the utility of boosters, especially against the omicron variant.
When the Science Is Messy: How SciCheck Handles Scientific Disputes

Many experts agree that we don’t know what the future will hold when it comes to the COVID-19 pandemic. In a piece explaining scientific fact-checking, E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, was quoted. “If there’s one thing we’ve learned through this pandemic, it’s to be humble about the virus. And to be very, very careful about making predictions.”
Six COVID-19 Mysteries Experts Hope to Unravel

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, was quoted discussing hybrid immunity and those who have not had COVID-19 yet. He noted that omicron as a first infection might not give people the immunity weapons that would be helpful later. “Omicron infection in previously unvaccinated, previously uninfected individuals seems to do quite poorly in inducing antibodies that can efficiently cross-neutralize other variants.”
Do You Need a Second COVID-19 Booster? ‘It Depends,’ Penn Medicine Experts Say

In a study published earlier this month, Penn Medicine researchers found that two doses of an mRNA COVID-19 vaccine generate significant antibodies. Though they wane over time, the researchers found that memory B cells are long lasting. E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, and one of the study’s authors, explained what this means for people eligible for another booster and the implications for others.
Q&A on Second COVID-19 Boosters for Older People

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, answered questions about the FDA’s approval for a second COVID-19 booster for older people. “I think having more options on the table for people is good. It gives physicians a little more choice and ease of recommending a fourth shot if they think it’s necessary,” Wherry said. But, he said, there is little to suggest that second boosters are needed for some of the eligible population.
Study Reveals How COVID-19 Infections Can Set Off Massive Inflammation in the Body

A new study published Wednesday in the journal Nature revealed that the SARS-CoV-2 virus can infect certain kinds of immune cells called monocytes and macrophages. “I think what was interesting about this is it could provide a clue and perhaps even some druggable targets for why some of the inflammation that we see in severe COVID-19 patients might get kick started the wrong way or proceed out of control,” said E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, who was not involved in the study.
Elizabeth Heller’s Lab Uncovers How Drug Addiction Can Create Lasting Changes in Genes

Elizabeth A Heller, PhD, speaks about uncovering a love of neurology, her unique research, and running a neuroscience lab throughout the pandemic.
Read More: Penn Medicine News Blog
April 2022
A Second COVID-19 Booster Can’t Hurt — But It May Not Help Much, Either
E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, spoke with The Atlantic about the FDA’s recent decision for Americans older than 50 to get a second booster shot. Wherry explained considerations to keep in mind.
The FDA Approves a Second Booster Shot for Adults 50 and Older

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, joined “Good Day Philadelphia” to discuss the newly authorized second booster COVID-19 vaccine and the new omicron subvariant BA.2.
Should You Get Another COVID-19 Booster?

The FDA has authorized additional COVID-19 shots for older Americans and those with certain immune deficiencies. E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, spoke about the news, and who needs the dose and when. “I’m a firm believer in vaccines. I like the idea of physicians and immunocompromised and high-risk patients having options,” Wherry said.
New York Times • Bloomberg • CBS3 • Associated Press • CBS News • KYW Newsradio • Boston Herald
Pfizer CEO Pushes Yearly Shots for COVID-19. Not So Fast, Experts Say.

On March 15, Pfizer shared it was seeking authorization of a second booster for people 65 and older, and Moderna on March 17 filed for a second booster shot for all adults — creating pressure for politicians and their scientific advisers to act. E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, was quoted.
Omicron Subvariant Could Become Dominant Strain in US
Health officials are keeping a close eye on the omicron subvariant that is behind a COVID-19 surge in parts of Europe and Asia. E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, is quoted.
COVID-19’s ‘Silver Lining’: Research Breakthroughs for Chronic Disease, Cancer, and the Common Flu

The billions of dollars invested in COVID-19 vaccines and research so far are expected to yield medical and scientific dividends for decades, helping doctors battle influenza, cancer, cystic fibrosis, and far more diseases. E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, was quoted, discussing research from the pandemic which represented a paradigm shift in immunology.
Our Antibodies Can Tell Us About Future COVID-19 Surges
While the coronavirus is tracked to see how it changes over time, experts discuss monitoring immunity too. Monitoring the status of our anti-disease protection would amount to a kind of immune surveillance that could tell us “when immunity wanes, and when it needs to be augmented,” explained E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology.
Pfizer and BioNTech Seek Authorization of a Second Booster Shot for Older Americans
Pfizer and BioNTech are seeking emergency authorization for a second booster shot of their coronavirus vaccine for adults 65 and older. The companies’ request is based on data from Israel, where such shots are authorized. But other studies have suggested that three doses of a vaccine are enough to protect most people for a long period of time. “We’re starting to see now diminishing returns on the number of additional doses,” said E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology.
New York Times • The Atlantic • KYW Newsradio
Remembering the COVID-19 Shutdown in Philadelphia Two Years Later

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, joined “Good Day Philadelphia” to discuss the pandemic since COVID-19 shut down Philadelphia two years ago and the latest with omicron’s subvariant.
The Coronavirus’s Next Move

Even if COVID-19 remakes itself many times, its offense will still knock up against some multilayered defenses. Slipping out of the grasp of antibodies isn’t that hard, but “just statistically speaking, I don’t think it’s possible to escape T-cell immunity,” explained E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, a contributor to a recent report that modeled various scenarios for the future with COVID-19.
March 2022
Experts Present Roadmap for the Next Phase of Living with COVID-19

A new report released Monday charts a path for the transition out of the COVID-19 pandemic, one that outlines both how the country can deal with the challenge of endemic COVID disease and how to prepare for future biosecurity threats. The roadmap was authored with input from Penn Medicine experts, including Ezekiel Emanuel, MD, PhD, vice provost for global initiatives, and E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology.
COVID-19 Booster Enhances Protection, Contrary to ‘Immune Fatigue’ Claims

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, spoke with FactCheck.org about the benefits of booster shots, after comedian Bill Maher incorrectly said COVID-19 boosters were “useless” and could cause “immune system fatigue.” Data show that people who have received booster shots are less likely to be infected with the coronavirus, even against the now-pervasive omicron variant. And there is no evidence that COVID-19 boosting can exhaust the immune system.
Does Exposure to Omicron Help Our Immunity, Even If We Don’t Get Sick?

If you’ve been dodging COVID-19, you might think your immune system is superhuman or you’re even immune to getting the coronavirus. But that’s not the case. If you’ve been wearing masks or social distancing, that’s providing protection, explained E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology. Even if you live with someone who is infected, your precautions might mean you aren’t exposed to a large enough dose of virus to cause an infection.
What the Omicron Wave Is Revealing About Human Immunity

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, and Scott Hensley, PhD, a professor of Microbiology, were quoted in a Nature article discussing the wealth of insights yielded by recent research into SARS-CoV-2. “We are just at the beginning of a wave of discovery,” Wherry said.
Should We Go All In on Omicron Vaccines?

While omicron-specific vaccines are in the works, experts have warned against trashing the original-recipe shots too soon, as we don’t know what the next major variant will look like. However, there is reason enough to avoid boosting in perpetuity with the original recipe. For the next round of COVID-19 shots, whenever they might be necessary, we may be better off using something else — an “insurance policy,” explained Rishi Goel, a PSOM student and research fellow at the lab of E. John Wherry, PhD, to help the body broaden its coronavirus scope.
Feb 2022
Is an Omicron Infection as Good as a Booster? What the Science Says About ‘Hybrid’ Immunity.
E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, spoke with the Philadelphia Inquirer about those who had omicron and what they should do about booster shots. Wherry discussed why people should never get infected on purpose, the immune system’s response to the vaccine, and how long to wait before getting a booster.
UK Report Did Not Find COVID-19 Vaccines Damage Immune Response

A video clip from a panel discussion on COVID-19 Monday is spreading on social media, misrepresenting what a report by U.K. health officials found. Multiple experts including E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, disputed the claim in the video that vaccines were doing damage. “It actually shows the vaccines are working to limit infection,” Wherry explained.
Will Omicron Leave Most of Us Immune?

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, spoke with The Atlantic about collective immunity, which is key to ending a pandemic. But its building blocks start with each individual. Allowing for shades of gray, a person’s current immune status hinges on “the number of exposures [to the spike protein], and time since last exposure,” Wherry said.
How Should We Be Using At-home Rapid Tests for Omicron?
E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, spoke with WHYY about rapid antigen tests and how they can used as a means of reducing omicron’s spread. “None of our measures of protecting ourselves or prevention are perfect,” said Wherry. “Vaccines aren’t perfect. Masks aren’t perfect. Tests aren’t perfect. But when used in combinations and in layers, we can dramatically reduce risk.”
Vaccines Provide Best Protection From COVID-19

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, discussed the latest on COVID-19, the omicron variant, and new research which concludes getting the vaccine is still the safest way to prevent COVID-19. “The bottom line message is that from symptomatic COVID-19 infection you do generate some immunity. But it’s still much safer to get your immunity from vaccination than from infection,” Wherry said.
Associated Press • FOX29 • Los Angeles Times
What Happens After Omicron? Four Key Questions About Where the Pandemic Goes Next
The omicron variant’s worldwide surge has upended early hopes for returns to normalcy and points to a more uncertain future for the pandemic, some experts say. “We are going to have a tremendous number of deaths among the unvaccinated,” said E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology. “And we’re going to have — even if we manage to eke our way through this — the scar tissue in the health system, which is going to last for a long time and is not going to be something that recovers when infection rates go down.”
Jan 2022
Expert Discusses Best Time to Use a COVID-19 Home Test Kit
Over the holidays, Americans flocked to stores to try to find at home COVID-19 tests kits. E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, recommended that if you’re using the home test as a precaution ahead of a gathering, test 6-12 hours before the event. “That’s going to make sure that when you’re with other people you’re at a low risk for transmitting.”
2021
Penn Medicine under John Wherry's leadership launches new Colton Center for Autoimmunity.

The Center, made possible through a $10 million gift from alumni Stewart and Judy Colton, unites game-changing research and patient care programs across the University, and connects Penn’s efforts to two other world-renowned institutions.
E. John Wherry, director of the Penn Institute for Immunology and chair of Systems Pharmacology and Translational Therapeutics in the Perelman School of Medicine, will serve as director of the new center. Under Wherry’s leadership, and in collaboration with a leadership council of Penn autoimmunity experts and advisory boards, the center will focus on driving four pillars: catalyzing development of therapies, cultivating rising stars, investing in people and big data tools, and collaborating across existing centers
New Studies Find Evidence of ‘Superhuman’ Immunity to COVID-19 in Some People

Recent research from E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, was highlighted in an NPR story about powerful immune responses against SARS-CoV-2. The research, published online in late August, showed that, over time, people who have had only two doses of the vaccine (and no prior infection) start to make more flexible antibodies — antibodies that can better recognize many of the variants of concern.
To Boost or Not to Boost?

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, and Aaron Richterman, MD, MPH, a fellow in the division of Infectious Diseases, were quoted in a piece explaining what COVID-19 booster shot studies say so far and why some are skeptical of the immediate need for boosters.
Debate Over Need for COVID-19 Boosters Continues

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, spoke with 6ABC about COVID-19 booster shots, noting that most research shows that vaccines are holding up right now, as they work to prevent severe illness, hospitalization, and death from COVID-19. That said, he does believe an extra dose is needed for some people. “If you are immunocompromised or have problems with your immune system, perhaps people of advanced age should be given priority for boosters now. For the general population of healthy adults, boosting people who are already vaccinated is not going to end the pandemic,” Wherry said.
Study Finds Pfizer, Moderna Shots Provide Protection in People with Multiple Sclerosis

There have been concerns about the efficacy of COVID-19 vaccines among immunocompromised people since clinical trials began last year. The immunocompromised are one of the most vulnerable groups to severe complications from COVID-19, but even with the extra stimulation from the vaccines, their immune systems still have trouble generating adequate levels of antibodies to fight the virus. People undergoing treatment for multiple sclerosis generate a strong T-cell response to the COVID-19 vaccines produced by Pfizer and Moderna despite having a muted antibody response, according to a new study by Penn researchers, including Amit Bar-Or, MD, FRCPC, director of the Center for Neuroinflammation and Experimental Therapeutics and chief of the Division of MS and Related Disorders, and E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology.
A Coronavirus Infection Might Not be Enough to Protect You

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, Perelman School of Medicine student Rishi Goel, and Beatrice Hahn, MD, a professor of Microbiology and Medicine, were quoted discussing how COVID-19 immunity differs between immunity from vaccination and from infection.
COVID-19 Vaccine Immunity Is Waning — How Much Does That Matter?

As debates about booster shots heat up, what’s known about the duration of vaccine-based immunity is still evolving. E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, and Jeffrey Morris, PhD, director of Biostatistics, were quoted discussing vaccine-induced immunity.
Pfizer Announces That COVID-19 Vaccine Works in Children Ages 5-11

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, joined “Good Day Philadelphia” to talk about the latest in coronavirus and COVID-19 vaccine news. Wherry discussed the recent announcement from Pfizer that its coronavirus vaccine has been shown to be safe and highly effective in young children aged 5 to 11 years.
COVID-19 After Being Fully Vaccinated

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, spoke with Buzzfeed about breakthrough COVID-19 cases, how the vaccines work to help protect one against the virus, and why it is important to get vaccinated — even if one is young and healthy. “These vaccines are absolutely still preventing severe disease, hospitalization, and death. Many of those mild cases we are seeing in vaccinated individuals would be much more severe if the individual had not been vaccinated,” Wherry explained.
Structure of the ancient TRPY1 channel from Saccharomyces cerevisiae reveals mechanisms of modulation by lipids and calcium

A team led by Vera Moiseenkova-Bell, PhD, a professor of Pharmacology and faculty director of the Electron Microscopy Resource Laboratory and Beckman Center for Cryo Electron Microscopy, used cryo electron microscopy — powerful imaging technology — to examine the structure of a TRPY1 channel, an ancient yeast protein. Transient Receptor Potential (TRP) channels span the outer membrane of many cell types to bind with molecules that guide cellular function. By understanding TRPs’ structure, one can manipulate how a cell communicates. Moiseenkova-Bell solved a structure of a yeast TRP channel which may benefit the wine industry, as this information could be used to manipulate fungal infections on grape vines. Cheers to that!
Robust T-Cell Response to mRNA COVID-19 Vaccines

mRNA COVID-19 vaccines provoke a swift and strong response by the immune system’s T cells — the heavy armor of the immune system — according to a study led by E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Institute for Immunology. The results revealed how the T-cell response to these vaccines unfolds and underline the importance of a second dose for people with no history of COVID-19. The findings showed, however, that in people with a history of COVID-19, the T-cell response was already robust after the first vaccine dose, with no significant increase after the second dose, which may have implications for potential future booster shots.
How Long Does COVID-19 Immunity Last Anyway?

COVID-19 vaccines are the best tool to keep people out of the hospital and alive. E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, spoke with NPR’s “Short Wave” about the impressive immune response from vaccines. His lab’s research shows that months after the vaccine, a person’s antibodies begin to become more powerful, more flexible. “So the same antibody can actually detect and, presumably, neutralize the Alpha variant, the Beta variant, and very likely the Delta variant as well,” Wherry said.
UNC Researchers Report a New Way to Charge CAR-T Against Solid Tumors

Avery Posey, PhD, an assistant professor of Systems Pharmacology and Translational Therapeutics, provided perspective on a recent study published in Nature Communications on CAR-T and solid tumors. He conveyed that the in vivo data is impressive; the approach was one of the next logical steps for CAR-T development, but it solves one of the problems for attacking solid tumors. Researchers still need to find safe and better targets.
Back to School During COVID-19

As students start to go back to schools, debates continue across the country on mask wearing. E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, joined Good Day Philadelphia to discuss the importance of wearing masks and what’s next for booster shots for immunocompromised patients.
COVID-19 Vaccine Booster Shots: What You Need to Know

Though research is continuing, early data using different methodologies suggests that immunity from the vaccines wanes at about eight months or earlier as the coronavirus’ Delta variant spreads. E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, explained the research behind recommendations for booster shots, booster shots for immunocompromised patients, and why attention should still focus on getting the unvaccinated vaccinated.
As COVID-19 Booster Shots Near, Penn Immunologist Explains Why He Hates the Term ‘Breakthrough Infection’

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, spoke with Philly Voice about growing research on the effectiveness of the mRNA COVID-19 vaccines and immune responses to those vaccines. Wherry’s team at Penn has closely examined the intricate details of the body’s immune response to a natural coronavirus infection and vaccination, accounting for multiple known variants. His lab studies not just the production of antibodies, but also the long-term blueprint for protection from memory B cells and T cells.
Study Details Robust T-cell Response to mRNA COVID-19 Vaccines, a More Durable Source of Protection

Messenger-RNA (mRNA) vaccines against the coronavirus that causes COVID-19 provoke a swift and strong response by the immune system’s T cells — the heavy armor of the immune system — according to a study from researchers at the Perelman School of Medicine. Although recent studies of vaccines tend to focus on the antibody response, the T-cell response is also an important and potentially more durable source of protection — yet little has been reported so far on the T-cell response to COVID-19 vaccines. In the study, published in the journal Immunity, senior author E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute of Immunology, shared that the findings underscore the need to look at T cells, not just antibodies, to understand the vaccine response for those who have not had COVID-19 and for those who have recovered from the disease.
Clarifying the Problem of T-Cell “Exhaustion”

Researchers have illuminated an important limitation of the immune system in prolonged battles against cancers or viruses: T cells, which are among the most powerful weapons in the immune systems of humans and other vertebrates, remain substantially programmed to stay exhausted even many weeks after exposure to a virus ended. “Exhaustion apparently leaves durable ‘epigenetic scars’ in T cells that constrain their ability to support an immune response. These findings point to a need to discover how to reverse that epigenetic scarring,” said study senior author E. John Wherry, PhD, chair of the department of Systems Pharmacology and Translational Therapeutics.
What Immunity Did Having COVID Give Me? Do I Need a Vaccine?

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, spoke with WHYY to answer listener and reader questions about those who have had COVID-19 and their immune response. Wherry discussed the benefits of the vaccine (as it provides more robust protection), protection from variants, and more.
Pfizer Wants To Give You a Booster Shot—but Experts Say It’s Too Soon

Many experts say it’s too soon for a COVID-19 booster when the vaccines work, and much of the world still hasn’t had its first shot yet. Data from lab studies and real-world infections indicate “the dam is holding,” said E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology. “Severe infections, hospitalizations, and deaths are being observed almost entirely in unvaccinated populations, even for the Delta variant.” And when infections do occur in people who have been vaccinated, the symptoms tend to be mild.
Why Philadelphians Should Worry About the Wildfires Out West

Smoke from wildfires has traveled across the country and settled over the Eastern Seaboard, resulting in air quality warnings that started in code orange. Trevor Penning, PhD, director of the Center of Excellence in Environmental Toxicology, was interviewed about the short- and potential long-term health risks that the polluted air poses for Philadelphians. “I think everyone needs to protect themselves to some extent,” he said.
The COVID-19 Vaccine Doesn’t Fully Protect People Like Me Who Are Immuno-compromised. Science Is Working on it.

A story about the uncertainty around the protection immuno-compromised cancer patients receive from the COVID-19 vaccine featured the writer’s oncologist Noelle Frey, MD, an associate professor of Hematology-Oncology. Alexander Huang, MD, an assistant professor of Hematology-Oncology, who recently published a study in Nature Medicine exploring how the immune system compensates when one set of immune cells are down, and Emily Blumberg, MD, a professor of Medicine and director of Transplant Infectious Diseases, were also featured.
Meme Spreads Falsehood About Vaccine Transfer Through Eating Meat

A new claim has emerged on Instagram suggesting that eating meat from animals vaccinated against COVID-19 could transfer the inoculation. “It just simply can’t happen,” said E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology. “It doesn’t work that way.” Referring to the messenger RNA vaccines from Moderna and Pfizer, Wherry explained that once the mRNA gets into a cell, it doesn’t propagate any further — meaning it doesn’t spread from one cell to another.
COVID-19 Vaccines Are Better Than We Ever Expected

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, was quoted discussing mRNA vaccines, which have emerged as the big winners in the pandemic — topping 90 percent effectiveness. “These will be among the most efficacious vaccines that we have. Period,” said Wherry.
Vaccine Protection May Diminish Need for Yearly Boosters

Scientists have found clues that the world’s leading COVID-19 vaccines offer lasting protection that could diminish the need for frequent booster shots, but they caution that more research is needed and that virus mutations are still a wild card. Critical studies are underway, and evidence is mounting that immunity from the mRNA vaccines does not depend exclusively on antibodies that dwindle over time. “I’m pretty optimistic. I wouldn’t rule out the need for boosters, but the immune response so far looks actually quite impressive,” said E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology.
Doctors Discuss Reasons Why People Aren’t Getting the COVID-19 Vaccine

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, joined “Good Day Philadelphia” to discuss some of the reasons why people say they aren’t getting the COVID-19 vaccine, and provide some medical insight into safety and effectiveness of the shots.
Body’s Second Line of Defense May Protect Against Coronavirus Variants

Cancer patients with impaired antibody responses were more likely to survive COVID-19 if they had stronger T cell responses, according to a recent study. “The bottom line is, yes, there is immunological evidence that [vaccines] are priming more than just neutralizing antibodies and that these other parts of the immune response are important,” said E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology.
How Do COVID-19 Vaccines Affect Immunocompromised People?

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, spoke with WHYY about the COVID-19 vaccine for those who are immunocompromised. “There’s some data from patients who have contracted COVID-19 that indicate that T cells do prevent or limit disease severity,” said Wherry. While some immunocompromised patients “won’t have perfect protection,” there is some hope that “maybe they won’t get sick if they get infected.”
Fact-Checking Anti-Vaccine Misinformation

Recent research from the Penn Institute of Immunology suggests vaccine side effects such as a sore arm, fever, or muscle aches could be a sign of a positive immune response and should not be a cause for concern. E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, noted that side effects “are not necessarily a bad thing — they may actually be an indicator of an even better immune response.”
I’ve Already Had COVID-19. Do I Need One Vaccine Shot or Two?

A recent study led by E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, found that people who were never infected with COVID-19 did not have a full immune response until after receiving the second dose. Wherry explained the study findings, noting that it’s very important that people who have never had COVID-19 get both doses of the Pfizer or Moderna vaccines, to get optimal high levels of antibodies. The Penn study did not show any evidence that a second dose could cause harm among those who have previously had COVID-19.
Debunking COVID-19 Conspiracy Theories That Could Hinder Vaccine Efforts

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, joined NBC10 to debunk three COVID-19 conspiracy theories that have some citizens hesitant about getting a coronavirus vaccine dose. For example, some falsely believe the mRNA vaccines could alter your genome or track you. “Just about every time you eat a meal, you’re ingesting RNA. This is not something that is really that unusual,” Wherry said.
Mask Mandate Relaxed

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, spoke about the new mask guidelines from the CDC. He notes we still have to be vigilant: “This is where we are today. As we see how things evolve under these new guidelines, we may be able to go further, or we may have to actually dial it back a little bit.”
Why Vaccine Side Effects Really Happen

Chills, headache, and fatigue after receiving a COVID-19 vaccine are perfectly normal. But reactions can vary wildly, and they don’t reflect how your immune system would respond to a COVID-19 infection. E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, spoke with National Geographic about why reactions to vaccines differ and the difference between side effects and adverse events.
Do People Who Have Had COVID-19 Need a Second Vaccine Shot?

A recent study suggests that there is a strong boost to the immunity of everyone who receives the first dose of an mRNA vaccine, including those who have previously had a SARS-CoV-2 infection. However, only people who have never had a SARS-CoV-2 infection appeared to benefit from the second dose. The research team, led by E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, tracked not only antibody responses to vaccination but also the creation of memory B cells, which provide longer lasting immunity against infection.
No COVID-19 Vaccine Side Effects? Why It’s Fine to Feel Fine

While side effects from the COVID-19 vaccine show your immune system is responding to the vaccine in a way that will protect against disease, evidence from clinical trials showed that people with few or no symptoms were also protected. However, there is some evidence of stronger immune response in those who get sick when vaccinated. A study led by E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, showed that people who reported side effects may have had somewhat higher levels of antibodies.
Vaccines Benefit Those Who Have Had COVID-19, Contrary to Viral Posts

The authorized COVID-19 vaccines have been found to be safe and effective in clinical trials and in real-world conditions, and there is no evidence showing that vaccinating those with previous SARS-CoV-2 could be unsafe. On the contrary, growing evidence shows one dose of the vaccine benefits individuals who’ve recovered from the infection, boosting their immune response. “Our study and several other studies show that there is a benefit, immunologically … in people who were previously infected,” said E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology.
FactCheck.org • Pharmacy Times
Dr. Wherry Discusses Johnson & Johnson Vaccine Resumption

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, joined Good Day Philadelphia to discuss the latest developments with the Johnson & Johnson COVID-19 vaccine, the importance of getting a second dose if you received an mRNA vaccine, and a recent COVID-19 outbreak at a Montgomery County School.
Indian Long Pepper Plant Packs Punch Against Glioblastoma in Animal Model

Piperlongumine, a chemical compound found in the Indian Long Pepper plant, is known to kill cancerous cells in many tumor types. Now an international team, which includes researchers at Penn, has illuminated one way in which the piperlongumine works in animal models — and has confirmed its strong activity against glioblastoma. Vera Moiseenkova-Bell, PhD, faculty director of the Electron Microscopy Resource Laboratory and Beckman Center for Cryo Electron Microscopy, was quoted.
Penn Medicine News Release • Genetic Engineering & Biotechnology News • News-Medical.Net
Researchers Detail More Cases of Clots Tied to COVID-19 Vaccines

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, discussed the decision to halt the Johnson & Johnson COVID-19 vaccine due to six cases of a rare blood-clotting disorder. “The chances of this happening to you are about between 1 and 100,000 to 1 in 1 million,” Wherry said. “If you’re an American, the chances of dying from COVID are 1 in 600.”
One Vaccine Dose May Be Enough For People Who Had COVID-19, Penn Research Shows

People who have already recovered from COVID-19 are showing signs of robust protection from the coronavirus and its variants after just one dose of the Pfizer or Moderna vaccines, according to a new Penn study published in Science Immunology. E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, spoke about the findings, including insights about variants and the development of possible booster shots.
Philly Voice • News-Medical.Net
Penn Medicine Studies How Long the COVID-19 Vaccines Last

As vaccinations were underway with the mRNA vaccines by Pfizer and Moderna, researchers at Penn began to test volunteers to better understand the vaccine immune response. They measured antibodies that show rapid immunity and memory B cells which indicate longer immunity. “What we were able to see is the vaccines produce really good memory B cells. Which means even if antibody levels fall lower, even if we might see variants that the antibodies may not catch well, we still have this second-tier defense,” said E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology.
Penn Scientists Discuss COVID-19 Vaccine Science and Policy

Drew Weissman, MD, PhD, a professor of Infectious Diseases, who played an integral role in the development of synthetic mRNA technology that is a critical component of the Pfizer/bioNTech and Moderna vaccines, E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics, and Jonathan Epstein, MD, executive vice dean and chief scientific officer of the Perelman School of Medicine, set out Monday to reassure the public that the vaccines are safe, effective, and rely on more than a decade of laboratory research on synthetic mRNA. They highlighted the science behind the vaccines during a virtual discussion. Steven Joffe, MD, MPH, interim chair of Medical Ethics & Health Policy, Holly Fernandez Lynch, JD, MBE, an assistant professor of Medical Ethics & Health Policy, and Susan Ellenberg, PhD, interim chair of Biostatistics, Epidemiology and Informatics, joined the discussion to talk about COVID-19 vaccine regulations and EUA policy.
PhillyVoice • Vox
Health Experts on the Future of COVID-19

As vaccines go into millions of arms, infectious disease experts consider what may happen to the virus in the long term. E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, was quoted, discussing why COVID-19 is likely here to stay and potential long-term outcomes based on vaccination efforts and potential variants.
COVID-19 Vaccines Are Entering Uncharted Immune Territor

Coronavirus vaccines have promised a return to a semblance of normal life. But they were not designed for, or tested extensively on, immunocompromised or immunosuppressed individuals. E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, was quoted discussing research which could help tailor future vaccines to immune systems that have been altered by drugs or disease, or that have simply aged out of maximal protection.
Penn joins ‘cryo revolution’ by adding Nobel-winning microscope

The Singh Center for Nanotechnology has added the newest technology to its arsenal of microscopes: the Krios G3i, a cryogenic electron microscope that will allow researchers to study cells, proteins, and engineered nanoparticles like never before. “Bringing this microscope onto campus is a big deal for everyone,” says Vera Moiseenkova-Bell of the Perelman School of Medicine.
Read More
Pandemic Precautions Made for an Illness-Free Year for Many. What That Means for Our Immune Systems.

Due to the social distancing, hand-scrubbing, and mask wearing that came along with the pandemic, there have been fewer cases of illnesses such as the flu and rhinovirus, a common cause of colds. As people look ahead towards the end of the pandemic, E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, explained what a return to the “real world” could mean for immune systems.
How Long Is the Vaccine Effective Is One of Many Questions Delaware Valley Residents Are Asking

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology, joined FOX29 to answer one of the biggest questions on people’s minds these days — just how long do the COVID-19 vaccines last? “Six months is kind of like the floor here. That is the minimum,” said Wherry. “Six months is about the longest data we have from a reasonable sized number of people we can draw conclusions.”
If You Don’t Have COVID-19 Vaccine Side Effects, Are You Still Protected?

Not having side effects, or having not as severe side effects, is no reason to worry when it comes to the COVID-19 vaccine, explained E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute for Immunology. While researchers do not fully understand why only some people have side effects from COVID-19 vaccines, the experience probably reflects the quirks of each person’s immune system more than it does the vaccine’s effectiveness, Wherry said.
Investigating COVID-19 Vaccine Immunity

A new study led by E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Immune Health Institute, is investigating how well the COVID-19 vaccines work in the real world. Wherry's team, profiled in The Philadelphia Inquirer, is measuring antibodies, various kinds of white blood cells, including “helper” T cells that can act as sentinels, marshaling support to fight an infection, and “killer” T cells that, as the name suggests, fight infection by killing cells that the virus has penetrated, as well as looking at how immunity is affected by virus variants.
Donald Trump’s COVID-19 Treatment: He Got Typical Drugs — Only Faster

President Trump’s therapies have been similar to those available to most other hospitalized COVID-19 patients — with two major exceptions. Regeneron has only been tried in about 2,000 people as part of a research trial, and the president has received everything far sooner than would a typical patient; most Americans hospitalized with COVID-19 are treated with Remdesivir. E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Institute for Immunology, was quoted.
Q&A on Coronavirus Vaccines

In the more than eight months since the novel coronavirus emerged and spread around the world, scientists across the globe have made rapid progress on developing a vaccine. E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Institute for Immunology, said that although there’s evidence that reinfection can occur, “it is likely unusual, if not rare,” and protective immunity “remains the more likely outcome of infection (and effective vaccination).”
Neanderthal Genes Linked to Severe COVID-19; Mosquitoes Cannot Transmit the Coronavirus

A new study led by E. John Wherry, PhD ,chair of Systems Pharmacology and Translational Therapeutics and director of the Institute for Immunology, may shed light on why some children develop the rare and dangerous multisystem inflammatory syndrome in children (MIS-C) after recovering from COVID-19, while most do not.
Deep Immune Profiling Shows Significant Immune Activation in Children with MIS-C

Taking the first deep dive into how the immune system is behaving in patients with multisystem inflammatory syndrome in children (MIS-C), research led by Laura Vella, MD, PhD, an assistant professor of Pediatrics, and E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute of Immunology, has found that children with this condition have highly activated immune systems that, in many ways, are more similar to those of adults with severe COVID-19.
Researchers Discover Potential Cause of Immunotherapy-related Neurotoxicity

New research led by Avery Posey, PhD, an assistant professor of Systems Pharmacology and Translational Therapeutics and a member of Penn’s Abramson Cancer Center, has uncovered the previously unknown presence of CD19 — a B cell molecule targeted by CAR T cell immunotherapy to treat leukemia, lymphoma, and multiple myeloma — in brain cells that protect the blood brain barrier. This discovery may potentially be the cause for neurotoxicity in patients undergoing CD19 directed CAR T cell immunotherapy.
Penn Medicine News Release • Medical Xpress • News-Medical.Net
Smell Could Be a Better Sign of Early COVID-19 Infection Than Fever

Because loss of smell is an early symptom of COVID-19 — and often the only symptom present in people who otherwise feel fine — it may be helpful in screening asymptomatic and pre-symptomatic carriers. “The idea is very attractive because we need testing any way we can get it, and there’s just not enough to go around. The other side of the equation is that people who wake up with allergies or a hangover and can’t smell the coffee as well as they did yesterday might panic and run to urgent care for a test. It would be good to understand the costs,” said E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Institute for Immunology.
Antibodies Fight Off the New Coronavirus, But What Do T Cells Do?

In a recent Nature Reviews Immunology article, research led by E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Institute for Immunology, summarized what scientists know about T cells and COVID-19 to date.
The Reinfection Question

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Institute for Immunology, joined NBC News to discuss recent coronavirus reinfection cases, the new Abbott rapid test, and more.
Taking Risks for Big Rewards

Much of the world has focused its attention on how T cells, which play a central role in immune response, might shape the trajectory of COVID-19 infection, and how immunotherapy can shed light on treatment of the disease. In this Q&A, Avery Posey, Jr., PhD, discusses how he hopes to leave an indelible mark on the world through scientific investigation.
Why ‘T Cell Immunity’ Won’t End the Coronavirus Pandemic

SARS-CoV-2 is one of seven coronaviruses known to infect humans, four of which are prevalent pretty much everywhere and cause colds and other respiratory infections. “Most people have been exposed [to a coronavirus] by early childhood,” said E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Institute for Immunology. But, he said, just because you have a T cell recognizing the coronavirus, that doesn’t mean SARS-CoV-2 still won’t make you sick.
What the Immune Response to the Coronavirus Says About the Prospects for a Vaccine

Sporadic accounts of reinfection — people recovering from COVID-19, only to fall ill and test positive again — have stoked fears that immunity to the novel coronavirus might be short-lived. E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Institute for Immunology, said, “We’re all hearing anecdotes, but I don’t know if any of us know what to think about them. So far, reports of reinfection have lacked sufficient information about the person’s immune responses to rule out other possibilities."
Coronavirus Vaccines and Immunity: What We Know

Although the pandemic still defies prediction, medical experts are expressing increasing optimism about the human immune system’s ability to fight the virus. A study led by E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Institute for Immunology, found that people’s T cell responses could be divided into three “immunotypes.” In the first type, T cell responses were “unbalanced” with an excess of helper cells and an emptying out of the ones that kill infected cells. The second type saw fewer helper cells and more killer ones. The last type largely lacked any T cell response, as if the immune system hadn’t even gotten started.
U.S. Far from Reaching Herd Immunity for COVID-19

The coronavirus has killed more than 750,000 people worldwide since late 2019, nearly a quarter of them in the United States. Rumors maintaining that the U.S. has reached herd immunity could push people to take unnecessary risks, leading to more infections and a worsening of the crisis. E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Institute for Immunology, was quoted.
Can You Get COVID-19 Twice? Scientists Say It’s Too Early to Tell

Recovery from the coronavirus seems to stimulate protective immunity, but there’s not enough data to determine how long that protection lasts. E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Institute for Immunology, was quoted.
Scientists Uncover Biological Signatures of the Worst COVID-19 Cases

Studies of patients with severe cases of COVID-19 show the immune system lacks its usual coordinated response. John Wherry, PhD,director of the Penn Institute of Immunology and chair of Systems Pharmacology and Translational Therapeutics, recently published a study of these telltale immune signatures. “A lot of these data are telling us that we need to be acting pretty early in this process,” Wherry said. As more findings come out, researchers may be able to begin testing the idea that “we can change the trajectory of disease.”
Penn Medicine News Release • New York Times
There’s Good News About Your Immune System and the Coronavirus

Antibodies aren’t the only tools the immune system has to fight repeat invaders like SARS-CoV-2. A new study led by E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute of Immunology, has shown that in addition to antibodies, people also develop virus-specific T cells.
What is SYNGAP1?

Dr. Elizabeth Heller was recently awarded a research grant award from the SynGAP Research Fund to support her lab’s work in epigenetic regulation of SynGAP1-related intellectual disability. With the SynGAP Research Fund’s award to support a postdoctoral fellow in the lab, Dr. Heller and her team will work to uncover druggable targets that could be used to develop a treatment for this rare genetic disorder. Congratulations, Dr. Heller, and many thanks to the team at the SynGAP Research Fund!
Why a COVID-19 Vaccine Will Be Hardest to Make for Those Most at Risk

COVID-19 has been shown to be much more deadly in older people, and a large part of that may have to do with the immune system. “Lack of response among some older people in the study could be linked to immunosenescence,” said Michael Betts, PhD, a professor of Microbiology, referring to a depletion of certain T- cells and the weakening of the frontline immune defense the body mounts against invading microbes. Betts and John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute of Immunology, are collaborating with others at Penn to study COVID-19’s effects on the immune system.
Hundreds petition Penn to extend widespread COVID-19 testing for the entire fall semester

Contrary to the petition, Paul Axelsen, Penn Med professor of Pharmacology, Biochemistry, Biophysics, and Medicine in the Infectious Diseases program, said widespread asymptomatic testing would not be useful, as the disease prevalence of COVID-19 off-campus is very low and will lend itself to false positive test results.
How the Coronavirus Short-Circuits the Immune System

In a disturbing parallel to H.I.V., the coronavirus can cause a depletion of important immune cells, recent studies Led by E. John Wherry, PhD and Lab.
NBC News Ask the Experts: Infections & Immunity

On a NBC News Google Hangout, E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute of Immunology, discussed his work investigating immune response to COVID-19, including his new study developing COVID-19 “immunotypes” and how treatments might be tailored to specific immune profiles in patients.
Congratulations to Dr. Pure!

Dr. Ellen Puré received a distinctive COVID-19 Pilot Award from the Penn Vet COVID Research Innovation Fund. The Fund, provided with critical start-up support through a gift from Vernon and Shirley Hill, will bolster Penn Vet’s rapidly expanding research and response program to fight the novel coronavirus.
- Ellen Puré, Grace Lansing Lambert Professor of Biomedical Science; Chair, Department of Biomedical Sciences, “Defining the Cellular and Molecular Basis of the Fibro-inflammatory Response to SARS-COV2 Infection”
COVID-19 management in light of the circadian clock

Circadian clocks control the function of our immune system, virus replication and the severity of infections. Our daily rhythms also regulate the pharmacokinetics and efficacy of several therapeutics. Consequently, better understanding of the effects of circadian biology on SARS-CoV-2 infection would improve the clinical management of COVID-19. Review on COVID-19 and the circadian clock by AK Reddy and his lab.
How the Coronavirus Short-Circuits the Immune System

In a disturbing parallel to H.I.V., the coronavirus can cause a depletion of important immune cells, recent studies found. John Wherry explains how the Coronavirus Short-Circuits the Immune System in this NYT article.
New “Blueprint” of Exhausted T Cell Lifespan Could Help Build Better Immunotherapies

In a new study published in Cell Press, the lab of E. John Wherry, PhD, chair of the department of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute of Immunology in the Perelman School of Medicine at the University of Pennsylvania, for the first time showed four key stages of so-called “exhausted” T cell development and the molecular mechanisms driving the transition from one stage to the next.
Penn’s Center of Excellence in Environmental Toxicology (CEET) Receives $8 Million Grant from the National Institute of Environmental Health Sciences

“The Center of Excellence in Environmental Toxicology combines rigorous scientific and medical research with direct community engagement and policy-making to effect positive outcomes for the health of our environment and our communities. One cannot conduct meaningful environmental health research without engaging the communities affected, ” said Trevor Penning, PhD, a professor of Systems Pharmacology and Translational Therapeutics and founding director of CEET.
How to Keep Your Immune System Healthy During the Coronavirus Pandemic, According to Experts

E. John Wherry, PhD, chair of Systems Pharmacology and Translational Therapeutics, told the Philadelphia Inquirer that supplements available for purchase will likely not be any help against COVID-19. There’s no evidence to suggest anything can boost your body’s defenses against this novel virus, he said.
Discovery of 318 novel loci for type-2 diabetes and related micro- and macrovascular outcomes among 1.4 million participants in a multi-ethnic meta-analysis

Fresh preprint out now! 40 loci (35 novel) assoc'ed with longitudinal bone accrual. Read More
Asbestos Exposure: Who Will Get Cancer?

Ian A. Blair, PhD, a professor of Systems Pharmacology and Translational Therapeutics, was interviewed about his search to discover biomarkers for asbestos exposure, as well as biomarkers that could give clues about the possible effects of those exposures. To date, nearly a dozen Philadelphia Schools have closed this year due to asbestos risks.
The dangers of asbestos: What the public should know

Marilyn Howarth and Ian Blair of the Perelman School of Medicine discuss the hazards of asbestos, how it harms the body, the asbestos crisis in the School District of Philadelphia, and why there is no safe level of asbestos. Homes, schools, and buildings built before 1980—the majority of structures in Philadelphia—have a higher risk of containing asbestos.
Congratulations to James H. Eberwine, Ph.D

On his impressive honor of being inducted into the National Academy of Medicine, for his pioneering work in the field of single-cell genomics that has revealed the complexities of human and mouse transcriptome variability. This is a great recognition of Jim’s impressive contributions to the field.
Sleep Deprivation Shuts Down Production of Essential Brain Proteins

Two studies in the recent issue of Science look at the important role synapses play in sleep.Akhilesh Reddy, MB, PhD, an associate professor of Pharmacology and not involved in either study, tells Scientific American that the research may help us understand how memories are processed while we sleep.
Congratulations to Dr. James Eberwine,

Recipient of the NIHDirector's Pioneer Award! Learn more Dr. Eberwine's project and research interests.
Getting “exhausted” T cells back into action against cancer

When a malignancy or chronic infection sets in, a kind of immune combat fatigue can follow. Finding ways to recharge immune cells can restore their ability to fight deadly diseases, says immunologist John Wherry.
Reviving Tired T Cells to Improve Immunotherapy Treatments

FierceBiotech highlighted a Nature paper by John Wherry, PhD, chair of Pharmacology and director of the Penn Institute of Immunology, and colleagues, which identified the protein TOX as key to waking up exhausted T cells.



